Medication Safety Risk Calculator
Assess Your Medication Risk
This tool estimates your risk of adverse drug reactions based on your health conditions and medications. The results are for informational purposes only and do not replace medical advice.
When you’re taking medication, you expect it to help - not hurt. But if you have one or more chronic health conditions, the risk of dangerous side effects goes up dramatically. It’s not just about the drug itself. It’s about how your body, already stretched thin by other illnesses, reacts to it. This isn’t rare. It’s the new normal for millions of people, especially as we age.
Why Existing Conditions Make Drugs More Dangerous
Your body doesn’t handle drugs the same way when you have diabetes, heart disease, kidney problems, or liver damage. These conditions change how your body absorbs, breaks down, and gets rid of medication. For example, liver disease can cut the activity of key enzymes by 30 to 50%. That means drugs like statins, antidepressants, or painkillers stick around longer in your system, building up to toxic levels even at normal doses. Kidney trouble does the same thing for drugs cleared through urine - like metformin, certain antibiotics, or blood thinners. If your kidneys aren’t filtering properly, those drugs pile up. The result? Higher chances of dizziness, confusion, bleeding, or even organ damage. This isn’t theory. A major study found patients with comorbidities were nearly three times more likely to have a serious adverse drug reaction than those without. In fact, two out of every three suspected drug reactions happened in people with multiple health issues. That’s not a coincidence. It’s a pattern.The Hidden Risk: Taking Too Many Pills
Most people with several chronic conditions end up on multiple medications. On average, adults over 65 with three or more illnesses take over four drugs a day. Nearly half take five or more. That’s called polypharmacy - and it’s where things get dangerous. Each new drug adds another chance for interaction. Some drugs compete for the same liver enzymes. Others lower blood pressure so much together that you faint. Some make your kidneys work harder, while others slow them down. The result? A 47% chance of at least one potentially harmful drug-drug interaction in elderly patients with multiple conditions. One in three of those interactions are major - meaning they could cause permanent harm or even death. Cancer patients face even higher risks. In one study of just 100 patients, 65 had dangerous drug interactions. Over a third were classified as major. And these aren’t just theoretical risks - they lead to real hospitalizations, longer stays, and extra costs of $1,200 to $2,500 per incident.Common Side Effects in People With Comorbidities
The side effects you see aren’t always the same as what’s listed on the pill bottle. In people with multiple health problems, the most common reactions are:- Weakness (36% of cases)
- Dizziness (12%)
- Headache (7%)
- Nausea and vomiting (combined 9%)
- Insomnia (3%)
High-Risk Comorbidities and Their Drug Traps
Some conditions are especially risky when paired with certain medications:- Heart disease + NSAIDs: Painkillers like ibuprofen can raise blood pressure and increase heart attack risk - especially if you’re already on blood thinners or diuretics.
- Diabetes + beta-blockers: These heart meds can hide low blood sugar symptoms. You might feel shaky or sweaty - but your heart rate won’t spike, so you won’t know you’re in danger.
- Liver disease + opioids: Your liver can’t break down pain meds properly. Even low doses can cause extreme drowsiness, breathing problems, or coma.
- Depression + SSRIs + blood thinners: Combining antidepressants with drugs like warfarin can increase bleeding risk by up to 50%.
- Chronic pain + opioids + alcohol: 77-93% of people in substance use treatment also smoke. Alcohol and opioids together slow breathing to dangerous levels.
Why Clinical Trials Don’t Tell the Whole Story
Most drug trials exclude people with multiple health problems. They want clean data - so they pick healthy volunteers or patients with just one condition. That means the safety data you see on the label doesn’t reflect real life. Up to 80% of elderly patients with three or more conditions were left out of the studies that approved their medications. So when your doctor says, “This drug is safe,” they’re relying on data that doesn’t include people like you. That’s why side effects you experience might not be listed anywhere. They’re real - but invisible to the system.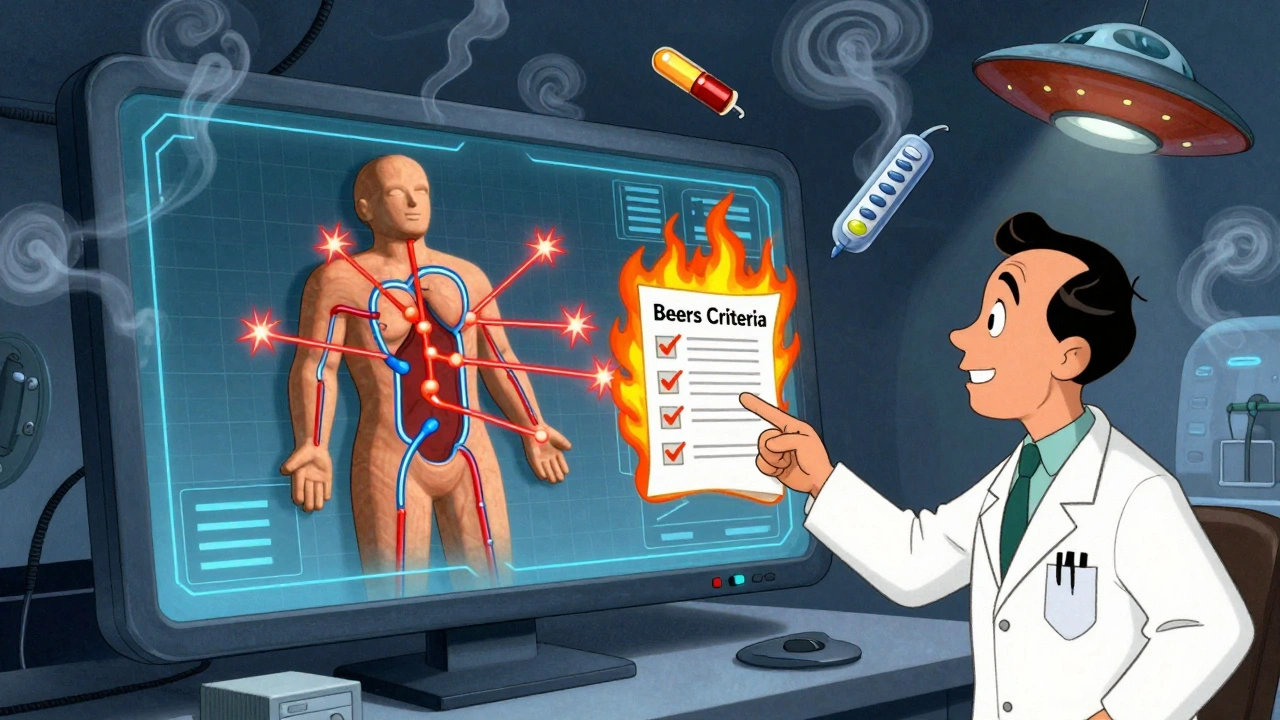
What Can You Do? Practical Steps to Stay Safe
You can’t control all the variables - but you can control how you manage your meds:- Get a full medication review. Ask your pharmacist or a clinical pharmacist to go through every pill, patch, and supplement you take. They’ll spot interactions your doctor might miss.
- Use a pill organizer with alerts. Taking the wrong dose or double-dosing is a common cause of reactions. Simple tools help.
- Track your symptoms. Keep a notebook: when you feel dizzy, weak, or nauseous - and what you took that day. Bring it to every appointment.
- Ask: “Is this still necessary?” Every year, review each medication. Can anything be stopped? Deprescribing isn’t giving up - it’s protecting yourself.
- Know your labs. If you’re on kidney- or liver-affecting drugs, ask for your GFR and liver enzyme results. A 30% drop in kidney function changes everything.
What’s Changing in Healthcare
The system is starting to catch up. Electronic health records now include comorbidity-aware alerts. If you have kidney disease, your doctor’s system might block certain drugs automatically. The FDA now requires drug makers to analyze how their medications affect patients with multiple conditions - up from 42% of applications in 2018 to 78% in 2023. New tools are emerging too. The NIH launched a public database in 2024 that tracks over 12 million patient records. It’s already flagged 217 new dangerous drug combinations. Machine learning models now predict ADRs with 89% accuracy - far better than old methods. And in pilot programs, doctors using real-time drug-risk scores - which adjust based on your latest blood work - have cut adverse reactions by over 30%.The Bottom Line
Having multiple health conditions doesn’t mean you can’t take medication. But it does mean you need to be smarter about it. The risks are real. The consequences can be severe. And the system isn’t always designed to protect you. The best defense? Be informed. Ask questions. Keep track. And don’t assume a prescription is safe just because it came from a doctor. Your body is more complex than the label lets on. Treat your meds like a team - not a checklist. And make sure every player knows how the others are playing.Can one chronic condition really make a drug more dangerous?
Yes. Even one chronic condition - like high blood pressure, diabetes, or liver disease - can change how your body processes medication. For example, liver disease can slow down how fast your body breaks down drugs, causing them to build up to toxic levels. Kidney problems can prevent drugs from being cleared from your system. These changes increase the risk of side effects, even at normal doses.
Is polypharmacy always dangerous?
Not always - but the risk goes up fast. Taking five or more medications increases your chance of harmful drug interactions by over three times compared to taking just one. The more drugs you take, the higher the chance one will interfere with another, or with your existing health condition. Many people need multiple meds, but each one should be regularly reviewed to make sure it’s still necessary.
Why aren’t these risks listed on drug labels?
Most drug trials exclude patients with multiple chronic conditions. The safety data on the label comes from studies done on healthier people. So side effects that happen in real-world patients - especially those with comorbidities - often don’t show up in official warnings. That’s why tracking your own symptoms and talking to your pharmacist is so important.
What medications are most risky for people with comorbidities?
Anticoagulants (like warfarin), antihypertensives (like beta-blockers), psychotropics (like SSRIs), and opioids are the top three high-risk classes. These drugs interact strongly with heart, liver, kidney, and mental health conditions. For example, combining SSRIs with blood thinners can increase bleeding risk by 50%. Always ask if your meds are on the Beers Criteria list - a guide to risky drugs for older adults.
How can I reduce my risk of adverse drug reactions?
Start with a full medication review with a pharmacist. Keep a symptom diary. Ask your doctor every year: “Can any of these drugs be stopped?” Use a pill organizer. Know your latest lab results - especially kidney and liver function. And never assume a new prescription is safe just because it’s from your doctor. Your health history changes how drugs work in your body.







Erin Nemo
Been there. My grandma was on 7 meds and started falling constantly. Turned out two of them were making her dizzy as hell. Pharmacist caught it in 10 minutes. Why do doctors just keep adding pills instead of removing?
James Allen
Oh wow, so now we’re blaming Big Pharma for not testing on people who actually need the drugs? Newsflash: clinical trials are expensive and regulated. If they included every diabetic, heart patient, and liver case, they’d never finish a study. You want safer meds? Stop demanding 15 different prescriptions and start taking responsibility for your health.
Also, the Beers Criteria? That’s a guideline, not a law. My uncle’s on an NSAID with heart disease and he’s fine. Stop fearmongering.
And yes, I know I’m the only one saying this - but maybe the problem isn’t the drugs, it’s the people who think they’re entitled to take 10 pills and still feel 20.
Rachel Stanton
Really appreciate this breakdown - especially the part about how side effects like weakness and dizziness get dismissed as ‘just aging.’ That’s so dangerous. Clinically, we call that ‘functional decline,’ and it’s often iatrogenic - meaning caused by the treatment itself.
One thing I always tell my patients: don’t just track symptoms - track timing. Did the dizziness start after adding the new beta-blocker? Write it down. Bring it in. Use the phrase ‘I suspect a drug interaction’ - it gets attention.
And yes, deprescribing is not failure. It’s precision medicine. Your body isn’t a vending machine - you can’t just keep inserting coins hoping for a different snack.
ariel nicholas
Let’s be clear: this isn’t about comorbidities - it’s about systemic collapse. The medical-industrial complex doesn’t want you healthy; it wants you perpetually medicated. Every drug trial excludes the elderly because they don’t fit the ‘ideal patient’ mold - which is code for ‘young, white, male, and healthy enough to be profitable.’
And don’t get me started on ‘pill organizers’ - as if a plastic box with 12 compartments is a solution to a $4 trillion healthcare crisis built on profit-driven polypharmacy.
Meanwhile, in countries with universal care, they’re cutting prescriptions, not adding them. We’re not broken because we have diabetes and hypertension - we’re broken because we’re treated like walking pharmacies.
And yes, I’m aware this is unpopular. But truth isn’t popular - it’s necessary.
Scotia Corley
While the article presents compelling data, it lacks structural nuance. The correlation between polypharmacy and adverse drug reactions is well-documented, yet the causal attribution remains ambiguous. Are interactions driven by pharmacokinetic factors, or are they a symptom of fragmented care delivery? The absence of a systems-level analysis weakens the argument.
Furthermore, the Beers Criteria, while useful, are not universally applicable. Regional prescribing patterns, genetic polymorphisms in CYP450 enzymes, and socioeconomic access to pharmacogenomic testing are omitted from the discussion. Without these, the recommendations risk being overly simplistic.
Debbie Naquin
Drugs aren't the enemy. The system is. We treat pills like magic bullets while ignoring the body as a whole system. When you break a bone, you don't just give painkillers - you set it. But with chronic illness? We just add more pills and call it treatment.
What if the real problem isn't the drugs, but the refusal to treat the person? The liver doesn't care about your diagnosis code. It just processes what you give it. And if you keep pouring poison into it - it's not the liver's fault it fails.
Maybe we need to stop asking how to make drugs safer and start asking how to make health less complicated.
Karandeep Singh
u s doctors are crazy give too many pills. in india we take 1 or 2 max. if you sick you go to doc and get better or die. no 10 pills a day. this is why people get sick from medicine not disease
Amber-Lynn Quinata
My mom died because of this. She was on warfarin and an SSRI. No one told her about the bleeding risk. The doctor said ‘it’s fine’ - but the label didn’t even mention it because her comorbidities weren’t in the trial. I’m so angry.
And now they want us to ‘track symptoms’ like it’s our job? Why isn’t the system doing this? Why do we have to be our own medical detectives?
😭 I just want to know my meds won’t kill me. Is that too much to ask?
amit kuamr
you think this is bad wait till you see what happens when you take meds with alcohol or weed. people dont care. they just want to feel good. the system is broken but so are the people using it
elizabeth muzichuk
So let me get this straight - we’re supposed to trust a system that excludes the elderly from trials, then tells us to ‘ask questions’ like we’re doctors? What about the 78-year-old widow who can’t afford to miss work to see a pharmacist? What about the ones who don’t speak English? What about the ones who are too tired to keep a diary?
This isn’t advice. It’s victim-blaming dressed up as empowerment.
And if you’re telling people to ‘deprescribe’ - fine. But who’s going to pay for the follow-up? Who’s going to be liable when someone stops a med and gets worse? The system doesn’t care. It just wants you to stop complaining and take your pills.
So no. I won’t be ‘proactive.’ I’ll be angry. And I won’t be alone.