Sleep Medication Selector Tool
This tool helps you determine which sleep medication might be most appropriate for your specific situation. Enter your details below to get a personalized recommendation.
Your Sleep Profile
Your Recommendation
Potential Side Effects
Quick Takeaways
- Trazodone is an atypical antidepressant often used off‑label for insomnia.
- Its sedative effect comes from serotonin antagonism, not the usual GABA pathway of many sleep drugs.
- Alternative agents fall into three buckets: classic hypnotics, other antidepressants with sedative properties, and antihistamine‑based sleepers.
- When choosing, weigh onset speed, next‑day grogginess, abuse potential, and interaction profile.
- For most patients, a short‑term trial of Trazodone (≤50 mg) works, but chronic insomnia often benefits from a tailored switch.
When doctors talk about a "sleep aid" they rarely mean a single magic pill. Trazodone is a serotonin‑modulating antidepressant that, at low doses, produces drowsiness and is therefore prescribed off‑label for insomnia. It was first approved by the FDA in 1981 for depression, but clinicians quickly discovered its nightly 0.5‑2 mg/kg dosing helps people fall asleep without the rebound effect seen in many benzodiazepines.
While Trazodone works for many, it isn’t the only option. This guide walks through the most common alternatives, compares key pharmacologic traits, and offers a practical framework for deciding which medication fits a particular sleep or mood profile.
What Makes Trazodone Unique?
Trazodone combines two mechanisms: serotonin‑type 2 (5‑HT2) receptor antagonism and weak serotonin reuptake inhibition. The 5‑HT2 blockade reduces cortical arousal, while the mild reuptake inhibition gives a subtle mood‑lifting effect. Because it doesn’t bind to GABA‑A receptors, it lacks the classic “benzo‑high” and has a relatively low abuse potential.
Typical insomnia dosing ranges from 25 mg to 100 mg taken 30 minutes before bedtime. Onset of sleep usually occurs within 30‑60 minutes, and the drug’s half‑life (6‑9 hours) means most patients experience minimal next‑day sedation-though higher doses can cause morning grogginess.
Why Look at Alternatives?
Several scenarios push clinicians toward another agent:
- Inadequate sleep onset or maintenance despite the maximum tolerated Trazodone dose.
- Significant daytime sedation, especially in the elderly.
- Concurrent depression or anxiety that requires a different antidepressant class.
- Drug‑drug interactions (e.g., CYP3A4 inhibitors) that raise Trazodone levels.
- Patient preference for a medication with a different side‑effect profile.
Understanding the trade‑offs across alternatives helps you avoid a trial‑and‑error approach.

Side‑by‑Side Comparison
| Medication | Primary Indication | Mechanism | Typical Nighttime Dose | Onset of Sleep | Half‑Life | Most Notable Side Effects |
|---|---|---|---|---|---|---|
| Trazodone | Insomnia (off‑label) | 5‑HT2 antagonist + weak SRI | 25‑100 mg | 30‑60 min | 6‑9 h | Dizziness, dry mouth, priapism (rare) |
| Zolpidem | Acute insomnia | GABA‑A positive modulator | 5‑10 mg | 15‑30 min | 2‑3 h | Complex sleep‑behaviour, next‑day drowsiness, dependence |
| Mirtazapine | Major depression, insomnia | α2‑adrenergic antagonist + H1 antihistamine | 15‑45 mg | 45‑60 min | 20‑40 h | Weight gain, sedation, dry mouth |
| Doxepin | Insomnia (low‑dose), depression | Tricyclic antidepressant, H1 antihistamine at low dose | 3‑6 mg | 60‑90 min | 15‑18 h | Anticholinergic effects, post‑ural dizziness |
| Sertraline | Depression, anxiety, OCD | Selective serotonin reuptake inhibitor (SSRI) | 50‑100 mg (evening off‑label use) | 1‑2 h | 26 h | GI upset, sexual dysfunction, insomnia (initial) |
| Diphenhydramine | OTC sleep aid | First‑generation antihistamine | 25‑50 mg | 30‑60 min | 4‑8 h | Morning hangover, anticholinergic load, tolerance |
Deep Dive into Each Alternative
1. Zolpidem (Ambien)
Belonging to the non‑benzodiazepine “Z‑drugs,” Zolpidem binds selectively to the ω1 subtype of the GABA‑A receptor. Its rapid onset makes it a go‑to for sleep‑onset insomnia, but the short half‑life can lead to complex sleep behaviours (e.g., sleepwalking). It’s Schedule IV in the U.S., reflecting modest abuse potential. Ideal for short‑term (<4 weeks) use in patients without a history of substance misuse.
2. Mirtazapine (Remeron)
Mirtazapine is an atypical antidepressant that blocks central α2‑adrenergic receptors, boosting norepinephrine and serotonin release, while also antagonising H1 histamine receptors. Its sedative effect is strongest at lower doses (15 mg), often prescribed to patients who need both mood lift and sleep. The trade‑off is weight gain and pronounced morning drowsiness at higher doses. It’s a solid choice for depressed patients with concurrent insomnia.
3. Doxepin (Silenor)
At doses ≤6 mg, Doxepin’s antihistaminic action dominates, providing a gentle sleep‑maintenance effect without the antidepressant side‑effects seen at higher doses. It’s FDA‑approved specifically for sleep maintenance insomnia. Because it’s a tricyclic, clinicians must watch for cardiac conduction issues, especially in older adults.
4. Sertraline (Zoloft)
Although primarily an SSRI, sertraline can be used off‑label in the evening to harness its mild sedative properties in patients whose anxiety worsens at night. The downside is the typical SSRI activation window-some users feel jittery before the sedative effect kicks in. It’s best when depression and anxiety predominate over pure insomnia.
5. Diphenhydramine (Benadryl) - OTC Option
First‑generation antihistamines like diphenhydramine cross the blood‑brain barrier and block H1 receptors, leading to noticeable drowsiness. It’s inexpensive and available without prescription, but tolerance builds quickly and anticholinergic load can be risky for seniors (confusion, urinary retention). Use only for occasional sleepless nights.
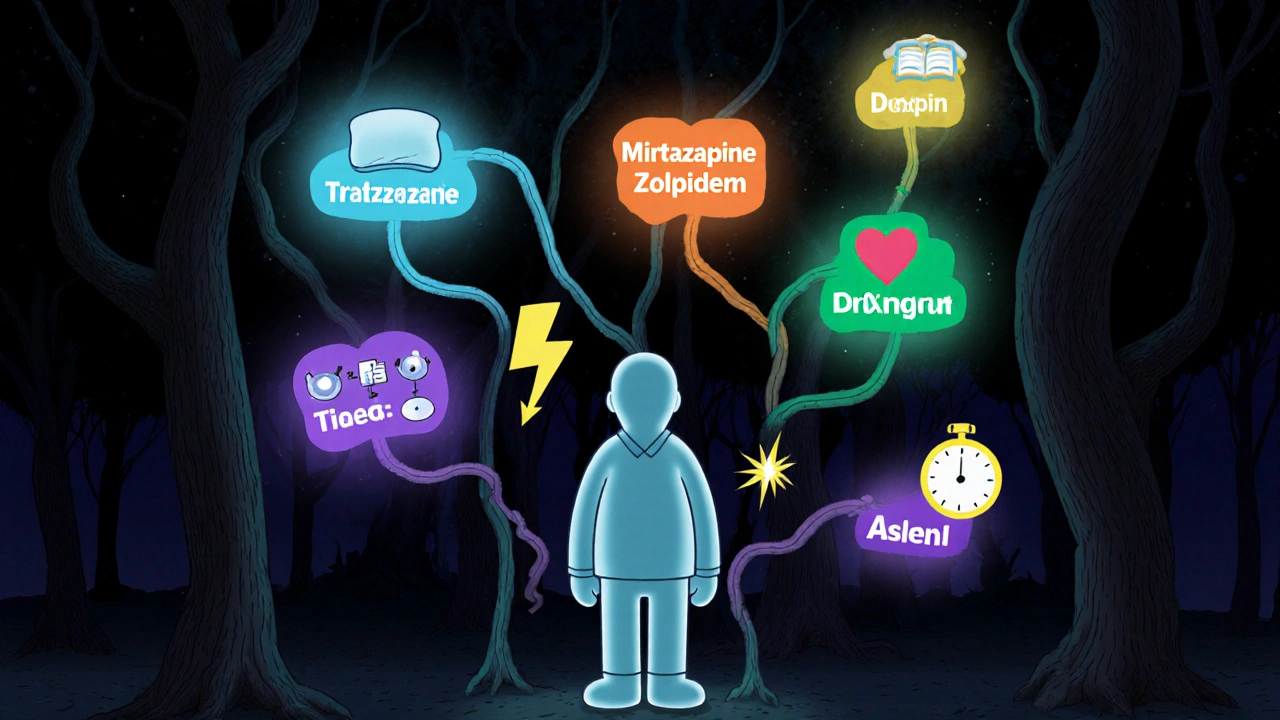
How to Choose the Right Agent
Think of medication selection as a decision tree:
- Primary problem? If insomnia is isolated, start with a short‑acting hypnotic (Zolpidem) or low‑dose Doxepin.
- Do you also need mood support? Opt for an antidepressant with sedative side‑effects (Mirtazapine or low‑dose Trazodone).
- Age and comorbidities? Elderly patients benefit from agents with low anticholinergic burden-avoid diphenhydramine and high‑dose Trazodone.
- Abuse risk? Skip Zolpidem if there’s a history of substance misuse; consider Trazodone or Doxepin, which have lower dependence potential.
- Drug interactions? Review CYP450 pathways. Trazodone and Zolpidem are metabolized by CYP3A4; strong inhibitors (ketoconazole, clarithromycin) can raise levels.
After you pick a candidate, start low, titrate slowly, and reassess after 2‑4 weeks. Document sleep latency, total sleep time, and daytime alertness to gauge efficacy.
Practical Tips & Common Pitfalls
- Never combine multiple sedatives. Mixing Trazodone with Zolpidem or diphenhydramine can cause profound respiratory depression.
- Take the medication **30 minutes before bedtime** and ensure a dark, screen‑free environment.
- Watch for **priapism** with Trazodone-though rare, it’s a medical emergency.
- For patients with **obstructive sleep apnea**, avoid high‑dose sedatives; consider non‑pharmacologic CBT‑I first.
- Educate patients that **sleep‑maintenance benefits may take 1‑2 weeks** to appear, especially with Doxepin.
Frequently Asked Questions
Is Trazodone safe for long‑term use?
Clinical guidelines suggest Trazodone is tolerable for months to years when used at low insomnia doses (25‑50 mg). Monitoring for daytime sedation, blood pressure changes, and rare priapism is advised.
Can I take Trazodone and an SSRI together?
Yes, the combo is common for patients with depression and insomnia. However, watch for serotonin syndrome signs (agitation, hyperreflexia) if doses are high.
How does low‑dose Doxepin differ from regular antidepressant doses?
At ≤6 mg, Doxepin’s antihistaminic effect predominates, providing sleep maintenance without the mood‑altering tricyclic effects seen at 75‑150 mg.
Why might a patient feel more awake after starting Trazodone?
A paradoxical activation can happen during the first week as the body adjusts to serotonin changes. This usually fades after 5‑7 days.
Are over‑the‑counter antihistamines a good substitute for Trazodone?
They work but develop tolerance quickly and carry anticholinergic risks, especially for older adults. Reserve them for occasional use.
Choosing the right sleep aid isn’t a one‑size‑fits‑all decision. By weighing onset speed, side‑effect profile, and any co‑existing mood disorder, you can move beyond trial‑and‑error and land on a medication that truly supports restful nights.





Manish Verma
Trazodone's unique serotonin profile makes it a solid choice for Aussie patients who need a non‑benzo sleep aid. Its 5‑HT2 antagonism cuts down cortical arousal without the classic GABA‑A high, so you avoid the typical hang‑over. At low doses it slips you into dreamland in about half an hour, and the half‑life means you’re rarely drowsy by breakfast. Compared with Z‑drugs it has a far lower abuse potential, which is something our healthcare system can’t afford to ignore. Bottom line: if you want a “quiet” night without feeding the pill‑pusher market, give trazodone a go.
Jennie Smith
Totally agree – it’s like hitting the sweet spot between a true sedative and a mood lift, especially when the patient’s already battling low‑grade depression. The colourful way it eases you into sleep feels almost artistic, like a gentle brushstroke rather than a thunderclap. Plus, the fact that it doesn’t leave you in a fog the next morning lets you stay motivated for the day ahead. I’ve seen mates swap out benzos for a modest dose of trazodone and notice a real boost in daytime energy. Keep spreading the word, this info really helps the community.
Greg Galivan
Trazodone’s dual mechanism can actually be a double‑edged sword if you don’t understand the pharmacology behind it. First, the 5‑HT2 receptor blockade reduces arousal, which is great for falling asleep, but it also interferes with the normal REM cycling that some people rely on for mental processing. Second, the weak serotonin reuptake inhibition can lift mood a bit, yet it may also trigger serotonin syndrome when combined with other serotonergic meds, something many prescribers overlook. The dosage window is narrow – 25 mg might be insufficient for a heavy‑set adult, while 100 mg can push you into morning grogginess that feels like a hangover without the alcohol. Metabolism through CYP3A4 means that common inhibitors like ketoconazole or even grapefruit juice can boost plasma levels unpredictably, leading to dizziness or rare priapism episodes that no one wants to talk about. In the elderly, renal clearance declines, so the drug sticks around longer and the risk of orthostatic hypotension climbs. Some clinicians habitually prescribe it off‑label for insomnia without addressing the underlying depression, which can mask symptoms and delay proper treatment. The literature shows that while short‑term trials (<4 weeks) improve sleep latency, long‑term use doesn’t necessarily sustain those gains and may even cause tolerance. When you compare it side‑by‑side with Z‑drugs, trazodone lacks the rapid on‑set (15‑30 min) that a night‑owl might crave, making it less suitable for abrupt night‑shift changes. However, its lower abuse potential is a huge win in populations vulnerable to dependency, like veterans or chronic pain patients. The side‑effect profile includes dry mouth, headache, and occasionally vivid dreams that can be unsettling, especially for people with PTSD. Switching to mirtazapine might be better for those who need both antidepressant and hypnotic effects, given its H1 antihistamine activity, but watch the weight gain. Conversely, low‑dose doxepin offers a more selective H1 blockade with minimal antidepressant action, ideal for maintenance insomnia. Ultimately, the decision hinges on a patient’s comorbidities, concurrent meds, and personal tolerance – there’s no one‑size‑fits‑all pill. So before you write a script, run through a checklist: dose, drug interactions, renal function, and the specific sleep problem you’re targeting. Only then can you harness trazodone’s benefits without stepping into the landmine of side‑effects.
Anurag Ranjan
Good points, Greg. Just add that checking CYP3A4 inhibitors is a quick safety step. Also, start low, go slow, especially in older adults.
James Doyle
From an ethical perspective, the indiscriminate off‑label use of trazodone raises serious concerns about the medical profession’s commitment to evidence‑based practice. When clinicians prioritize convenience over rigorous risk‑benefit analysis, they inadvertently perpetuate a culture of pharmaceutical complacency. The pharmacodynamic intricacies-5‑HT2 antagonism coupled with weak SRI activity-demand a nuanced appreciation that many primary‑care prescribers lack, leading to suboptimal patient outcomes. Moreover, the potential for iatrogenic serotonin excess, especially in polypharmacy scenarios, underscores the necessity for interdisciplinary oversight. In health systems already strained by cost constraints, resorting to a “one‑pill‑fits‑all” approach ignores the sophisticated therapeutic algorithms that have been painstakingly developed over decades. It is incumbent upon us, as stewards of patient welfare, to champion individualized regimens rather than defaulting to the lowest‑effort prescription. The comparative data clearly show that alternatives such as low‑dose doxepin or mirtazapine may offer superior side‑effect profiles for certain demographics, which should inform formulary decisions. Ultimately, safeguarding patients from avoidable adverse events is not merely a clinical imperative but a moral one.
Edward Brown
yeah you nailed the ethics angle but i think the conspiracy is that pharma pushes trazodone because it’s cheap and easy to market it as a sleep aid while hiding the priapism risk it’s rarely talked about in the pamphlets we get at the pharmacy the whole system is rigged to downplay those rare but scary side effects
ALBERT HENDERSHOT JR.
Excellent discussion, everyone. It’s clear that a thoughtful, patient‑centered approach is essential when considering trazodone or any alternative. 🌟 By weighing onset time, half‑life, interaction potential, and individual comorbidities, clinicians can tailor therapy to each person’s unique sleep architecture. Remember to monitor for daytime sedation and adjust the dose gradually. Keep sharing evidence‑based insights – it raises the standard of care for all.
Cheyanne Moxley
Wow Albert, you really think a smiley face fixes everything? This isn’t a self‑help blog, it’s serious med talk. People struggle with insomnia, and we need hard facts, not feel‑good vibes. Drop the coaching act and give us raw data, please.
Kevin Stratton
Sleep science is never one‑size‑fits‑all.