Swelling in your ankles, puffy face, or sudden weight gain over a few days? It might not be just salt or a bad day. Sometimes, the culprit isn’t your diet-it’s a medication you’re taking. Fluid retention, or edema, is a common but often overlooked side effect of many everyday drugs. If you’ve noticed your rings don’t fit, your shoes feel tighter, or your legs feel heavy without explanation, it’s time to look at what’s in your medicine cabinet.
How Fluid Retention Actually Works
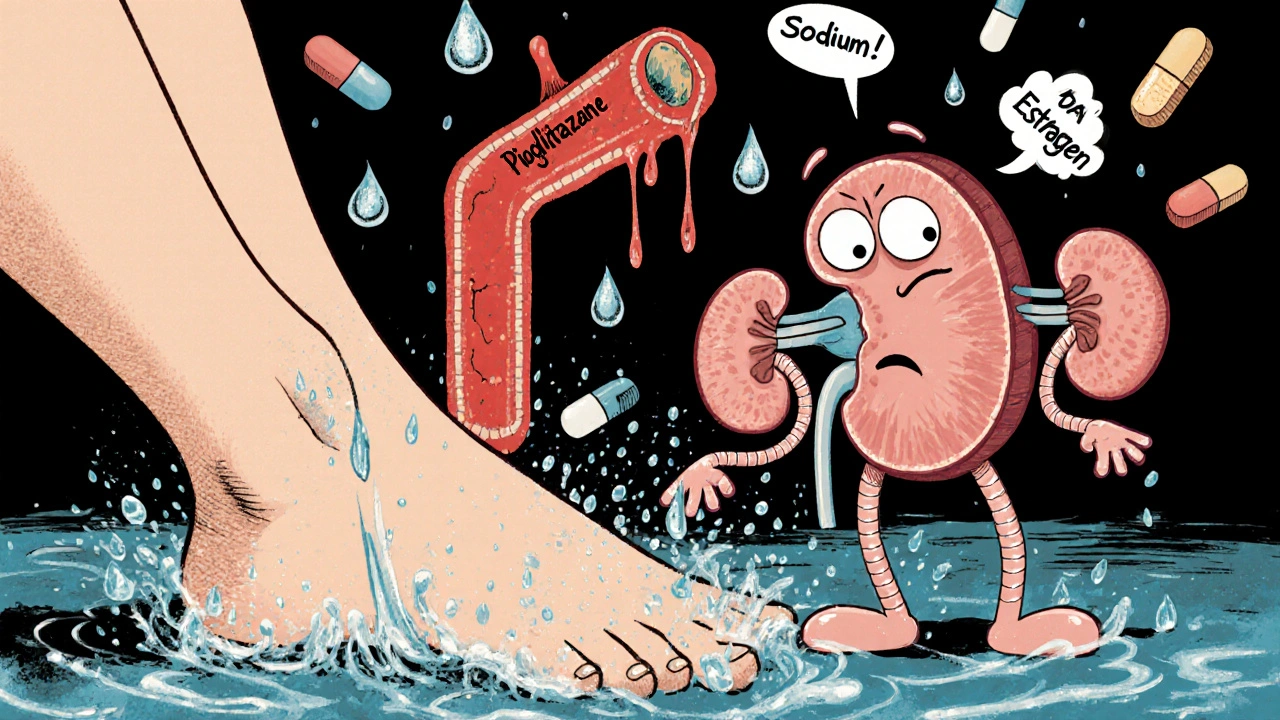
Your body keeps a tight balance of fluids. Kidneys filter blood, remove excess water, and send it out as urine. But some drugs mess with that system. They might make your kidneys hold onto sodium, which pulls water with it. Or they could weaken blood vessel walls, letting fluid leak into surrounding tissues. The result? Swelling in your feet, hands, or belly. It’s not always obvious at first-maybe just a 2-pound gain over a week. But if it keeps climbing, it’s a signal.
Common Medications That Cause Fluid Retention
Not all drugs cause this. But a surprising number do. Here are the most common ones you might be taking right now.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen, naproxen, and celecoxib. These are common for headaches, arthritis, or menstrual pain. But they reduce kidney blood flow, causing sodium and water to build up. A 2023 study in Annals of Internal Medicine found that regular NSAID users had a 40% higher chance of developing noticeable edema compared to non-users.
- Calcium channel blockers such as amlodipine, nifedipine, and diltiazem. These are prescribed for high blood pressure and angina. They relax blood vessels-but sometimes that relaxation lets fluid escape into tissues, especially around the ankles. Up to 1 in 5 people on these drugs report swelling, especially after being on them for months.
- Thiazolidinediones like pioglitazone and rosiglitazone. Used for type 2 diabetes, these help insulin work better. But they also activate receptors in fat and kidney cells that cause water retention. Patients on these often gain 2-5 kilograms in the first few months, mostly from fluid, not fat.
- Estrogen-containing medications, including birth control pills and hormone replacement therapy. Estrogen increases production of renin and aldosterone, hormones that tell your kidneys to hold onto salt and water. Women on these often notice swelling before their period, but it can become constant if the dose is too high.
- Corticosteroids like prednisone and hydrocortisone. Used for inflammation, asthma, or autoimmune conditions, these drugs alter electrolyte balance. They can cause rapid fluid buildup-sometimes 3-5 kilograms in just a few days. This is especially common in older adults or those with heart or kidney issues.
- Some antidepressants, particularly tricyclics like amitriptyline and SSRIs like sertraline. These affect neurotransmitters that influence kidney function. While not as common, fluid retention shows up in about 10% of long-term users, especially when combined with other medications.
Who’s Most at Risk?
Not everyone on these drugs will get swollen ankles. But some people are more likely to. Risk goes up if you:
- Are over 65 years old
- Have heart failure, kidney disease, or liver cirrhosis
- Are pregnant or have a history of preeclampsia
- Take more than one medication that causes fluid retention
- Have high sodium intake alongside your meds
If you have any of these conditions and are on one of the drugs above, your doctor should monitor you more closely. A simple blood test for sodium, potassium, and creatinine can show if your kidneys are struggling to manage fluid.
What to Do If You Notice Swelling
Don’t panic. But don’t ignore it either. Here’s what to do step by step.
- Check your weight daily. Weigh yourself at the same time each morning, after using the bathroom and before eating. A gain of more than 1-2 kilograms in 2-3 days is a red flag.
- Look for patterns. Does the swelling get worse after you take your pill? Does it improve when you’re active or elevate your legs? Keep a simple log for a week.
- Reduce salt. Even if you’re already eating low-sodium, cut back further for 5-7 days. Avoid processed foods, canned soups, soy sauce, and restaurant meals. See if the swelling eases.
- Elevate your legs. When sitting, put your feet up on a stool. This helps gravity move fluid back toward your heart.
- Don’t stop your meds. Never quit a prescription on your own. Some of these drugs are critical for your health. Instead, talk to your doctor or pharmacist.
When to See a Doctor
Call your doctor if:
- Swelling spreads to your belly, chest, or face
- You feel short of breath, especially when lying down
- Your skin over the swollen area feels tight, shiny, or leaves a dent when you press it (pitting edema)
- You have chest pain, rapid heartbeat, or confusion
These could mean fluid is building up in your lungs or around your heart-a sign of worsening heart or kidney failure. This isn’t just an inconvenience. It can be dangerous.
Alternatives and Adjustments
Your doctor might not take you off the drug entirely. Often, they’ll adjust the dose, switch you to a different class, or add a diuretic.
For example:
- If you’re on a calcium channel blocker and getting ankle swelling, your doctor might switch you to an ACE inhibitor or ARB-these often reduce swelling instead of causing it.
- If you’re on an NSAID for arthritis, they might suggest acetaminophen or a topical gel instead.
- If you’re on a thiazolidinedione and gaining weight, metformin or a GLP-1 agonist might be a better fit for your diabetes.
For people on estrogen therapy, switching to a lower-dose pill or a non-hormonal option like a progesterone IUD can help. And if you’re on prednisone, your doctor may try to lower the dose over time or use it only during flare-ups.

What You Can Do Right Now
Here’s a quick checklist you can use today:
- Look at your medicine list. Do you take any of the drugs mentioned above?
- Have you gained weight without changing your diet or activity?
- Do your shoes feel tighter? Do your rings pinch?
- Is the swelling worse at the end of the day?
If you answered yes to any of these, write down your meds and symptoms. Bring it to your next appointment. Don’t wait for your next check-up. If you’re on multiple medications, ask your pharmacist for a medication review-they spot these interactions all the time.
Fluid Retention Isn’t Always Harmful-But It’s a Warning Sign
Some swelling is harmless. A little puffiness after standing all day, or during menstruation, is normal. But when it’s tied to a drug you’ve been taking for weeks or months, it’s your body telling you something’s off. Medications save lives-but they also carry hidden trade-offs. The goal isn’t to avoid treatment. It’s to use it wisely.
By paying attention to small changes in your body, you can catch problems early. And with the right adjustments, you can stay healthy without unnecessary swelling.
Can over-the-counter painkillers cause fluid retention?
Yes, common OTC painkillers like ibuprofen, naproxen, and diclofenac can cause fluid retention. They work by blocking enzymes that help your kidneys remove sodium. Even short-term use can lead to noticeable swelling in people who are sensitive, especially if they already have high blood pressure or kidney issues. Acetaminophen is a safer alternative for pain relief if fluid retention is a concern.
Will drinking more water help with medication-induced swelling?
No, drinking more water won’t fix it-and it might make it worse. Fluid retention isn’t caused by dehydration. It’s caused by your body holding onto water because of how the drug affects your kidneys or blood vessels. Drinking extra water doesn’t flush it out. In fact, it can increase pressure in your tissues. The key is reducing sodium and talking to your doctor about adjusting your meds.
Can fluid retention from meds lead to long-term damage?
If left unchecked, yes. Chronic fluid buildup can increase pressure on your heart, worsen existing heart failure, or strain your kidneys. It can also lead to skin breakdown, infections, or blood clots in swollen limbs. The swelling itself isn’t always the problem-it’s what it’s hiding. That’s why it’s important to address it early, not just treat the symptom.
Are natural diuretics like dandelion or green tea safe to use with these meds?
Not without checking with your doctor first. Natural diuretics can interact with prescription drugs. For example, dandelion can increase the effect of lithium or diuretics, leading to dangerous drops in potassium. Green tea can interfere with blood pressure meds. What seems harmless can create new risks. Always talk to your pharmacist before adding supplements.
How long does it take for swelling to go away after stopping the medication?
It depends on the drug and your body. For NSAIDs, swelling often starts to fade within 2-5 days after stopping. For calcium channel blockers or corticosteroids, it can take 1-3 weeks. Diuretics may be prescribed temporarily to help flush out excess fluid. But never stop a medication without medical advice-even if the swelling bothers you.
Next Steps: What to Do Today
Take five minutes right now. Look at your medicine cabinet. Write down every prescription, OTC pill, and supplement you take daily. Check each one against the list above. If you see a match and you’ve noticed swelling, make an appointment. Don’t wait for symptoms to get worse. A simple conversation with your doctor or pharmacist could prevent bigger problems down the road.









Don Angel
Man, I just realized my ankles have been puffier since I started taking ibuprofen for my back... I thought it was just aging, but now I'm scared. I'm gonna check my meds list tonight.
Alex Boozan
Fluid retention is a classic pharmacokinetic artifact resulting from renal sodium reabsorption mediated by COX-2 inhibition and vasodilatory dysregulation. Stop blaming diet. The system is rigged.
mithun mohanta
Oh wow, I'm so relieved I'm not the only one who's been looking like a balloon after my diabetes med kickstarted. Pioglitazone? More like piogli-BOOM. My shoes are now fashion statements. I'm not gaining weight-I'm just... expanding my aesthetic.
Evan Brady
Here’s the thing no one tells you: if you're on a calcium channel blocker and your socks leave indentations like a prison tattoo, it’s not laziness-it’s pharmacology. I’ve seen patients go from 160 to 175 in two weeks and swear they’re eating salad. It’s the drug. Not the donuts. Swap to an ARB if you can. Your ankles will thank you. And yes, elevating your legs works-try it while watching Netflix. Gravity’s a free therapist.
Ram tech
why do u even take meds anyway? just eat less salt and stop being weak. my grandpa took 12 pills and still ran marathons. u just lazy.
Jenny Lee
Just checked my meds-yep, amlodipine. My shoes have been tight for weeks. Time to call my doc. Thanks for the wake-up call.
Jeff Hakojarvi
Hey, I know this can feel scary-but you're not alone. I had this exact thing with prednisone after my autoimmune flare. It felt like I was turning into a water balloon. What helped? Daily weigh-ins, cutting out the soy sauce, and asking my doc about a short diuretic course. You’re not overreacting-you're being smart. Keep going. And if you're nervous about talking to your doctor, write down your symptoms first. I did. It made me feel way more in control.
Timothy Uchechukwu
Western medicine is a scam. In Nigeria we just drink ginger tea and pray. Your kidneys don't need fixing they need faith. Why do you trust a pill more than your ancestors?
Ancel Fortuin
Of course the pills cause swelling. The pharmaceutical lobby owns the FDA. They want you bloated so you need more drugs. Diuretics? That's just another product line. They're not helping you-they're harvesting your fear. Wake up. The real cure is organic kale and sunlight. And maybe a tinfoil hat.
Hannah Blower
Let’s be honest-this isn’t about medication. It’s about your entire relationship with your body. You’ve outsourced your physiology to Big Pharma and now you’re shocked when your body rebels? Fluid retention is your soul screaming for autonomy. You want to fix it? Stop taking pills. Start taking responsibility. And maybe read some Foucault. Power doesn’t just live in prescriptions-it lives in your passive compliance.
Gregory Gonzalez
Wow. A whole article about swelling. And not one mention of the fact that 87% of people who report this are also on Instagram. Coincidence? Or is the real culprit the algorithm that makes you feel bad about your legs?
Ronald Stenger
Fluid retention? That's just what happens when you let the government tell you what to take. I stopped all meds after 2016. My blood pressure's fine. My ankles? Never looked better. America needs to break free from the pharmaceutical cartel. You think your doctor cares? They're paid by the pill.