When you’re pregnant, your body changes in ways you never expected. One of the most surprising? Your pancreas suddenly has to work three times harder. That’s because the placenta starts pumping out hormones that block insulin - your body’s natural way of keeping blood sugar in check. For about 1 in 10 pregnant women, this leads to gestational diabetes - high blood sugar that shows up during pregnancy and usually disappears after birth. But left unmanaged, it can lead to big problems: a baby weighing over 9 pounds, shoulder injuries during delivery, low blood sugar in the newborn, or even preeclampsia for the mother. The good news? With the right tools, most women bring their numbers back into range and have healthy pregnancies - just like those without diabetes.
What Your Blood Sugar Numbers Should Be
If you’re diagnosed with gestational diabetes, you’ll get a target range for your blood sugar. These aren’t guesses - they’re based on years of research showing what keeps both mom and baby safest. The American Diabetes Association says:
- Fasting or before meals: under 95 mg/dL (5.3 mmol/L)
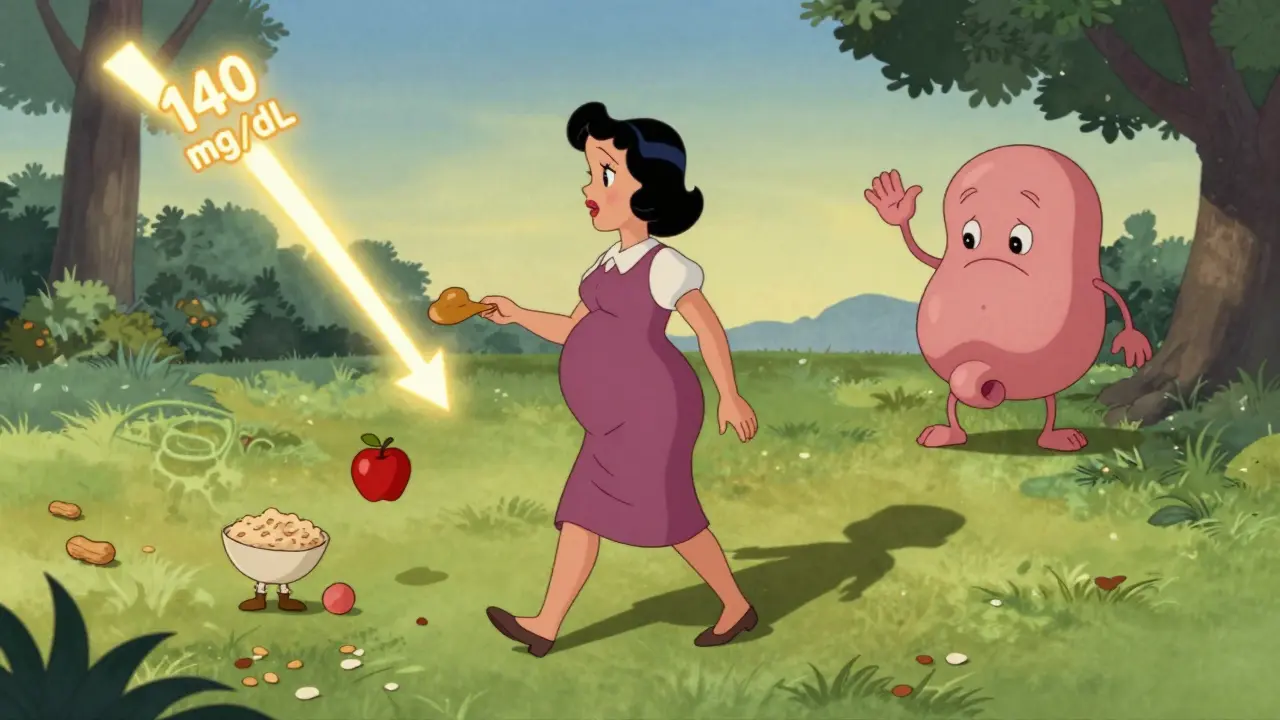
- One hour after eating: under 140 mg/dL (7.8 mmol/L)
- Two hours after eating: under 120 mg/dL (6.7 mmol/L)
Some clinics use even tighter goals, especially if you’ve had complications before. You’ll check your levels with a simple finger prick test, usually 4 to 6 times a day - before breakfast, after each meal, and sometimes at bedtime. Writing down what you ate and your numbers helps spot patterns. Maybe your blood sugar spikes after oatmeal but stays steady after eggs. That’s information you can use.
Continuous glucose monitors (CGMs) are becoming more common, especially for women who’ve had Type 1 diabetes before. Studies show they cut the risk of having a very large baby by nearly 40% and reduce severe low blood sugar in newborns by more than half. Even if you don’t use one, knowing your targets and checking regularly is the single biggest factor in a healthy outcome.
Food Is Your First Treatment
Most women - about 70 to 85% - control their gestational diabetes with food alone. No pills. No shots. Just smarter eating. The key isn’t cutting carbs entirely. It’s spreading them out and pairing them with protein and fat to slow down how fast they hit your bloodstream.
Here’s how it works in practice:
- Three meals a day, plus two to three small snacks
- Each meal has about 45 grams of carbs - that’s one cup of cooked rice, two slices of whole grain bread, or three-quarters of a cup of oatmeal
- Snacks should have 15 to 30 grams of carbs, paired with protein: an apple with peanut butter, plain yogurt with a handful of nuts, or cheese with whole grain crackers
- Carbs make up only 35-40% of your daily calories. The rest comes from healthy fats (avocado, olive oil, salmon) and lean protein (chicken, tofu, eggs)
One simple trick that works for most women: eat your protein first, then vegetables, then carbs. A UCSF Health survey found this order lowers post-meal spikes by 25 to 40 points. Why? Protein and fiber slow digestion. Your body doesn’t get hit with a sugar rush.
Portion control matters more than you think. A cup of pasta looks small, but it’s three carb choices (45 grams). Use measuring cups at first. You’ll get better over time. Apps like MyFitnessPal help track carbs, but don’t obsess. Aim for consistency, not perfection.
Move Your Body - Even Just a Little
Exercise isn’t optional. It’s medicine. Walking for 30 minutes after meals can drop your blood sugar by 20 to 30 mg/dL. That’s the same effect as some medications - without the side effects.
What works best? Brisk walking, swimming, stationary cycling, or prenatal yoga. You don’t need to run a marathon. Just get moving. Many women find morning walks help lower fasting glucose - the stubborn high numbers you wake up with. One Reddit user shared that her fasting numbers dropped 15 to 25 points after daily 20-minute walks. That’s huge.
Try to walk 15 to 30 minutes after breakfast, lunch, and dinner. Even if you’re tired, even if you’ve been nauseous - get up and move. It’s one of the most effective, free tools you have.
When Diet and Exercise Aren’t Enough
Some women still can’t hit their targets. That’s not your fault. It just means your body needs extra help. About 15 to 30% of women with gestational diabetes need insulin. And that’s okay.
Insulin doesn’t cross the placenta. It doesn’t affect the baby. It just helps your body do what it can’t on its own. Many women fear needles, but the pens are tiny, the needles are fine, and most people get used to them within days. Your doctor or diabetes educator will show you how. You’ll learn to adjust doses based on your food and activity - and your numbers will start to stabilize.
Some providers offer metformin, an oral pill. But it’s not the first choice. Studies show about 30% of women on metformin still end up needing insulin anyway. And while it’s safe for the baby, long-term data on children is still being studied. So insulin remains the gold standard when you need it.
Fasting Glucose Is the Trickiest Part
If you’re waking up with high blood sugar, you’re not alone. Nearly half of women with gestational diabetes struggle with this. It’s not because you ate too much the night before. It’s because your liver is releasing stored sugar while you sleep - a normal process that gets exaggerated by pregnancy hormones.
The fix? A bedtime snack. Not a big one. Just 15 grams of carbs with a little protein. Think: 6 whole grain crackers with 1 ounce of cheese, or half a cup of cottage cheese with a few berries. This tells your liver, “We’ve got fuel. Don’t release more.” Many women see their morning numbers drop within days.
What Happens After the Baby Is Born
After delivery, your blood sugar usually returns to normal. That’s good news. But here’s the catch: 50% of women who had gestational diabetes will develop Type 2 diabetes within 10 years. That’s not inevitable - but it’s a warning.
Right after birth, you’ll get a glucose test 6 to 12 weeks later. If it’s normal, you still need to be screened every two years. If it’s high, you may already have Type 2 diabetes - and you’ll need to start managing it.
The best way to prevent it? Lose 5 to 7% of your body weight after pregnancy and keep moving. The TODAY2 study showed that women who did this cut their risk of Type 2 diabetes by 58% over 15 years. That’s more powerful than any drug.

Emotional Support Matters Too
Getting diagnosed with gestational diabetes can feel scary. You might feel guilty, overwhelmed, or even ashamed. You’re not alone. A survey of 1,200 women found that 68% felt emotional distress after diagnosis. Forty-two percent were anxious about insulin.
But here’s what most women say later: “I wish I’d known how manageable this was.” With good education, support, and a clear plan, most women feel in control again within weeks. Talk to a certified diabetes educator. Join a group like DiabetesSisters or Reddit’s r/GestationalDiabetes. You’ll find people who’ve been there - and they’ll tell you it gets easier.
One of the most common complaints? Conflicting advice. One doctor says eat 45 grams of carbs per meal. Another says 30. Stick with one provider or dietitian you trust. Don’t jump between opinions. Consistency beats confusion.
What Not to Do
There are some mistakes that make managing gestational diabetes harder:
- Skipping meals to “save carbs” - this makes fasting sugar worse
- Drinking fruit juice or sweetened drinks - even “natural” ones spike blood sugar fast
- Waiting too long to start monitoring - if you’re diagnosed at 28 weeks, you’ve already missed the window to prevent complications
- Checking glucose less than four times a day - women who check fewer times have more than double the risk of NICU admission
Don’t try to tough it out. This isn’t about willpower. It’s about science. The numbers don’t lie. And your baby deserves the best start possible.
You’ve Got This
Gestational diabetes isn’t a failure. It’s a sign your body is doing its best under new conditions. With the right tools - smart eating, daily movement, regular checks, and support - you can manage it completely. And you’ll give your baby a healthier start, protect your own long-term health, and prove to yourself that you’re stronger than you think.
Can gestational diabetes go away after pregnancy?
Yes, in about 70% of cases, blood sugar returns to normal after delivery. But you still need a follow-up glucose test 6 to 12 weeks after birth to confirm. Even if your numbers are normal, you’re at higher risk for Type 2 diabetes later, so regular screening every two years is essential.
Will my baby be born with diabetes?
No, babies are not born with diabetes because of gestational diabetes. But high blood sugar in the womb can cause the baby to produce extra insulin, leading to low blood sugar after birth. That’s why newborns of mothers with uncontrolled GDM are monitored closely right after delivery. With good management, this risk drops dramatically.
Do I need to take insulin if I have gestational diabetes?
Not everyone does. About 70-85% of women control their blood sugar with diet and exercise alone. If your numbers stay high after a few weeks, your provider may recommend insulin. It’s safe for your baby and often the most effective option. Needles sound scary, but most women adapt quickly and find them easier than expected.
Can I eat fruit with gestational diabetes?
Yes, but choose wisely and watch portions. Berries, apples, pears, and oranges are better than bananas, grapes, or mangoes. Always pair fruit with protein or fat - like a handful of almonds or a spoon of Greek yogurt. This slows sugar absorption. One small piece of fruit (about 15g carbs) per snack is usually fine.
What’s the best time to exercise during pregnancy with gestational diabetes?
The best time is 15 to 30 minutes after eating. Walking after meals helps lower blood sugar spikes caused by food. Many women find morning walks help reduce fasting numbers. Aim for 30 minutes, five days a week. Even short 10-minute walks after snacks help. Consistency matters more than intensity.
How often should I check my blood sugar?
Most providers recommend checking four to six times a day: fasting in the morning, and one or two hours after each meal. Some also check at bedtime. Checking less than four times daily increases the risk of complications. Record your numbers with what you ate - this helps your provider spot patterns and adjust your plan.
Is gestational diabetes my fault?
Absolutely not. Gestational diabetes happens because of hormones your body makes during pregnancy - not because of what you ate or how much you weighed before. It’s not caused by poor choices. Many healthy, active women get it. It’s a common condition that affects up to 1 in 10 pregnancies. What matters now is how you manage it - not why it happened.
What should I eat for breakfast with gestational diabetes?
Avoid cereal, toast, or fruit juice - they spike blood sugar fast. Instead, try: scrambled eggs with spinach and avocado, Greek yogurt with chia seeds and a few berries, or cottage cheese with sliced almonds. Keep carbs under 30 grams per breakfast and always include protein and fat. This keeps your morning numbers stable.







Catherine Scutt
Ugh, I hate how everyone acts like gestational diabetes is just a ‘little hiccup.’ My OB told me to ‘eat less sugar’ like I was some kind of toddler. I checked my numbers for 3 weeks and still got flagged. Turns out, my body just hates pregnancy. No amount of kale smoothies fixed it. Insulin saved my sanity.
Angela Stanton
Let’s break this down statistically: the ADA targets are based on the HAPO study (2008), which showed a linear correlation between maternal glucose and fetal adiposity. Anything above 95 fasting = exponential risk increase in LGA neonates. CGMs reduce NICU admissions by 42% (JAMA 2021). If you’re not using one, you’re essentially flying blind. Also, ‘natural’ fruit juice? That’s just liquid candy with a wellness veneer. 🍎❌
Kiruthiga Udayakumar
My cousin in India had GDM and she ate rice every day with ghee. No insulin. No stress. Just walked 45 mins after dinner. Your Western obsession with ‘carb counting’ is ridiculous. We’ve been feeding pregnant women for centuries without glucose monitors. Stop overcomplicating it. 🌾❤️
Patty Walters
Just wanted to say-eating protein first? LIFE CHANGER. I was hitting 180 after lunch until I started with eggs, then spinach, THEN the sweet potato. Down to 110 in 3 days. Also, don’t stress if you miss a check. I forgot twice and my doc didn’t even blink. Just get back on track. You’re doing better than you think. 💪
Phil Kemling
It’s fascinating how medicine frames GDM as a ‘problem to be solved’ rather than a physiological adaptation. Your body isn’t broken-it’s optimizing for fetal development in a nutrient-rich, insulin-resistant environment. The real tragedy isn’t high glucose. It’s that we’ve turned pregnancy into a metrics-driven surveillance state. Maybe the numbers aren’t the enemy. Maybe our fear of imperfection is.
tali murah
Oh please. You ‘managed’ it with ‘food’? That’s like saying you ‘managed’ a hurricane by wearing a raincoat. You’re lucky your baby didn’t come out the size of a watermelon. And now you’re gonna act like it’s no big deal? 🙄 I’ve seen the NICU reports. Your ‘healthy pregnancy’ is just a 5-star Yelp review on a life-threatening condition. #GDMisntAGoodLook
Diana Stoyanova
Y’ALL. I had GDM and thought I was doomed. Then I started walking after EVERY meal-even if it was just 10 mins around the living room. My fasting went from 110 to 85 in 2 weeks. I cried the first time I saw a green number. I started a TikTok called ‘GDM Walk Squad’ and now we have 12k followers. You’re not alone. Your body is not your enemy. Movement is medicine. And yes, you CAN eat fruit-just not with your morning toast. Pair it. Always. 🍓🚶♀️✨
Jenci Spradlin
Bedtime snack? YES. Half cup cottage cheese + 3 strawberries. That’s it. I was waking up at 140. Now I’m at 88. No insulin. Just snack. Also, don’t trust your doctor’s ‘normal’ range if it’s not matching your glucometer. Mine was off by 15 points. Bought a new one. Game over. 💯
Elisha Muwanga
Why are we letting American doctors dictate pregnancy nutrition? In my country, we eat whole grains, dairy, and meat. No carb counting. No monitors. No fear. This obsession with numbers is a capitalist healthcare scam. You’re being sold a product: the glucose meter. The truth? Most women manage fine with traditional diets. Stop buying into the fear.
Maggie Noe
I love how this post says ‘you’ve got this’ like it’s a motivational poster. But what if you’re terrified of needles? What if you’re exhausted and nauseous and your partner thinks you’re being dramatic? I needed insulin. I cried every time I injected. But I did it. And my daughter is 3 now-perfectly healthy. So yes. You’ve got this. Even when you feel like you don’t. 🤍
Gregory Clayton
OMG I JUST REALIZED-I was eating oatmeal for breakfast like a total idiot. I thought it was ‘healthy.’ Turns out it’s basically sugar paste. I switched to eggs and avocado and my fasting dropped 40 points. I feel like a genius. Also, why is no one talking about how the ‘no fruit juice’ rule is the only thing keeping me from screaming? 🍊💀
Pooja Kumari
I just want to say-I was diagnosed at 32 weeks and felt like the worst mom ever. I cried every time I saw my numbers. I thought I ruined my baby’s life. But then I found a group of women who shared their stories-some on insulin, some not, some with big babies, some with tiny ones. We didn’t fix each other. We just held space. And now? My daughter is 18 months old. She’s laughing, chubby, and healthy. GDM didn’t define me. My love did. And yours will too. ❤️