When your kidneys start leaking protein into your urine, it’s not just a lab result-it’s a warning sign your body is under serious stress. For people with diabetes, this leak-called albuminuria-is often the very first sign of diabetic kidney disease (DKD). And here’s the hard truth: if you ignore it, your kidneys could fail. But the good news? Catching it early and acting fast can stop or even reverse the damage.
What Is Albuminuria, and Why Does It Matter?
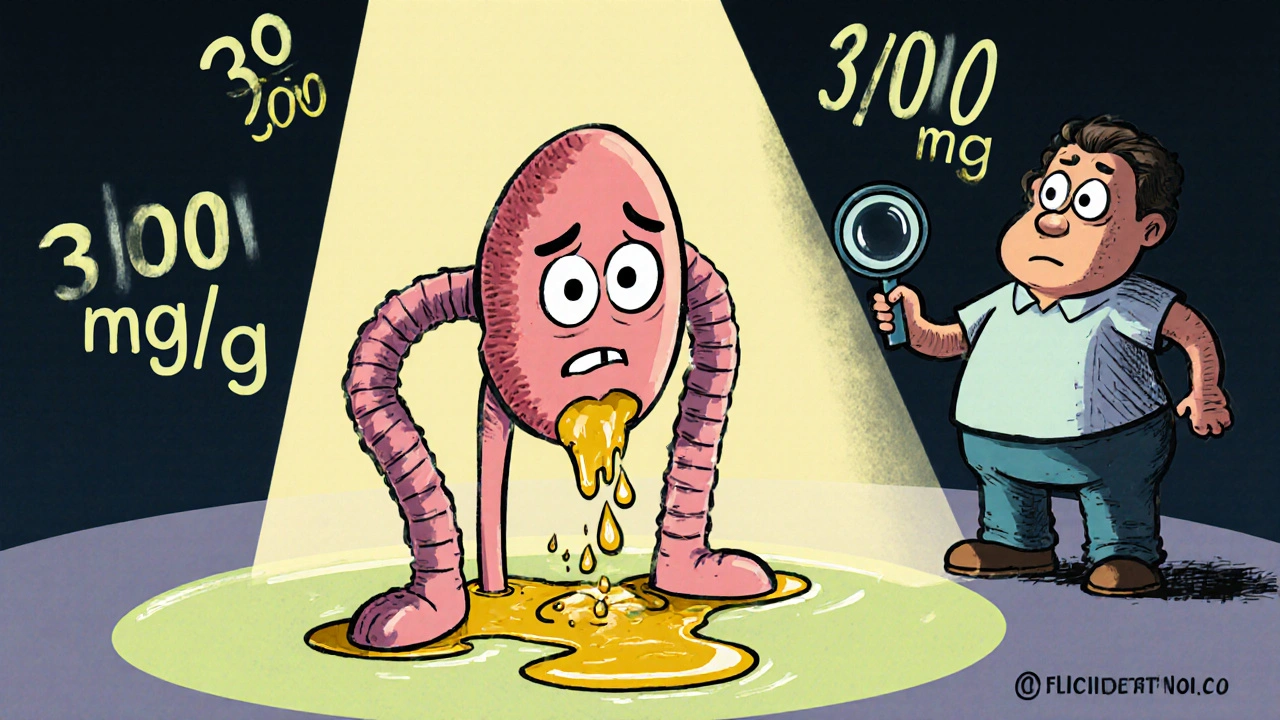
Albumin is a protein your kidneys normally keep in your blood. When they’re healthy, they don’t let it escape into your urine. But when high blood sugar damages the tiny filters in your kidneys, albumin slips through. That’s albuminuria. The modern definition is simple:- Normal: less than 30 mg of albumin per gram of creatinine (UACR <30 mg/g)
- Moderately increased: 30 to 300 mg/g (formerly called microalbuminuria)
- Severely increased: more than 300 mg/g (formerly macroalbuminuria)
The term "microalbuminuria" was dropped in 2012 because even small amounts of albumin in urine mean kidney damage is already happening. There’s no safe level. Any rise above 30 mg/g is a red flag.
And it’s not just about the kidneys. People with albuminuria above 300 mg/g have a 73% higher risk of dying from any cause-and an 81% higher risk of dying from heart disease-compared to those with normal levels. Your kidneys are telling you your whole body is in danger.
How Do Doctors Diagnose It?
You can’t feel albuminuria. No swelling. No pain. That’s why testing is non-negotiable.The standard test is a urine albumin-to-creatinine ratio (UACR). It’s done on a simple spot urine sample-no need to collect for 24 hours. But one high result doesn’t mean you have DKD. Albumin levels can spike temporarily from:
- Intense exercise in the last 24 hours
- Fevers or infections
- High blood sugar over 300 mg/dL
- Severe high blood pressure (over 180/110 mmHg)
- Menstruation
That’s why guidelines require two out of three abnormal tests within 3 to 6 months before confirming a diagnosis. If your first test shows 80 mg/g, don’t panic. Retest. But if it stays high, you need a plan.
Annual UACR screening is a Class A recommendation from the American Diabetes Association-meaning it’s backed by the strongest evidence. For people with type 2 diabetes, testing should start at diagnosis. For type 1 diabetes, begin after 5 years of disease.
Yet in real life, only 58-65% of clinics actually do this test every year. Why? Many don’t have electronic reminders built into their systems. Patients forget to bring samples. And some providers still don’t realize how powerful this simple test is.
Tight Glycemic Control: The Foundation of Prevention
The most powerful tool you have against DKD? Keeping your blood sugar under control.The landmark DCCT/EDIC study followed over 1,400 people with type 1 diabetes for more than 30 years. Those who kept their HbA1c below 7% had:
- 39% lower chance of developing microalbuminuria
- 54% lower chance of developing proteinuria
The best part? Those benefits lasted decades-even after some people’s blood sugar control slipped. This is called "metabolic memory." Your body remembers the good control you had early on.
For type 2 diabetes, the UKPDS study found that every 1% drop in HbA1c reduces your risk of kidney disease by 21%. That’s huge.
Today, the ADA recommends:
- HbA1c under 7% for most adults with diabetes
- HbA1c under 6.5% if you’re newly diagnosed, young, and at low risk for low blood sugar
- More lenient targets (like 7.5-8%) if you’re older, have other health problems, or struggle with hypoglycemia
But here’s the gap: only 52.5% of U.S. adults with diabetes hit that 7% target. And even fewer-just 12.2%-control their blood sugar, blood pressure, and cholesterol all at once. That’s why DKD keeps rising.
Blood Pressure: The Second Pillar of Protection
High blood pressure doesn’t just strain your heart-it crushes your kidneys. And in DKD, the two feed each other.For years, doctors aimed for 130/80 mmHg. But newer data changed that.
The SPRINT trial showed that pushing systolic pressure below 120 mmHg reduced albuminuria by 39%. Sounds great, right? But it also increased the risk of sudden kidney injury. For every 47 people treated this hard, one had harm.
So current guidelines are smarter:
- KDIGO recommends <120/80 mmHg only if your UACR is above 300 mg/g and you’re at high risk
- ADA recommends <140/90 mmHg for most people with DKD
That doesn’t mean you shouldn’t aim lower. But aggressive targets need careful monitoring. Your doctor should check your potassium and kidney function every few weeks when starting or increasing blood pressure meds.
Medications That Protect Your Kidneys
If you have albuminuria, you’re not just treating blood sugar and blood pressure-you’re fighting for your kidneys with specific drugs.RAAS inhibitors (ACE inhibitors or ARBs) are the first-line defense. They don’t just lower blood pressure-they directly protect the kidney’s filters. The IRMA-2 trial showed that losartan (100 mg/day) cut progression from micro- to macroalbuminuria by 53%. The key? Use the maximum approved dose, even if your blood pressure is normal. That’s the goal: reduce albuminuria, not just pressure.
Then come the newer stars:
- SGLT2 inhibitors (like empagliflozin, dapagliflozin): These drugs make your kidneys flush out extra sugar. But they also reduce kidney stress. The 2023 EMPA-KIDNEY trial showed they cut the risk of kidney failure by 28% in patients with UACR ≥200 mg/g.
- Finerenone: A new non-steroidal mineralocorticoid blocker. In trials, it lowered UACR by 32% in just 4 months and slowed kidney decline by 23% over three years-even when patients were already on maximum ACE/ARB therapy.
Together, these drugs form a powerful trio. But here’s the shocking part: only 28.7% of patients with DKD get all three recommended therapies. Why? Cost. Access. Lack of awareness. And too many doctors still treat each condition in isolation.
What Happens If You Don’t Act?
Albuminuria is a progression marker. Once you’re in the moderately increased range (30-300 mg/g), your risk of kidney failure rises sharply. If you reach severely increased (over 300 mg/g), you’re at high risk of needing dialysis within 10-15 years.But here’s the flip side: if you can reduce your UACR by 30% or more within the first year of treatment, your risk of kidney failure drops by nearly half. That’s not just a statistic-it’s your life.
Studies show that people who get their UACR below 300 mg/g cut their risk of heart attack, stroke, and death by 34-41%. Your kidneys aren’t just a filter-they’re a warning system for your entire body.
Real-World Barriers and How to Overcome Them
Knowing what to do is one thing. Doing it consistently is another.Patients miss urine tests because:
- They don’t know they need to do it
- They forget to bring a sample
- They’re embarrassed or confused about how to collect it
Doctors miss opportunities because:
- Electronic health records don’t flag when UACR is overdue
- They don’t know how to titrate RAAS inhibitors to full dose
- They don’t refer patients to nephrologists early enough
But some clinics are fixing this.
- One hospital system added automatic UACR alerts in their EHR. Testing rates jumped from 60% to 92%.
- Another started offering point-of-care urine testing in the exam room. Patients were 37% less likely to drop out of follow-up.
- Pharmacists now manage medication dosing in 30% of diabetes clinics. They get 89% of patients to the full, protective dose of ACE/ARBs.
You don’t need a perfect system. You need to start. Ask your doctor: "When was my last UACR test?" If you don’t know, schedule one now.
What You Can Do Today
If you have diabetes, here’s your action plan:- Ask for your UACR result. Don’t wait for your doctor to bring it up.
- If your result is above 30 mg/g, ask: "What’s my next step?" Don’t accept "We’ll watch it."
- Get your HbA1c tested every 3 months. Aim for under 7%.
- If you’re on blood pressure meds, ask if they’re ACE inhibitors or ARBs. If not, ask why.
- If you’re on metformin, ask if an SGLT2 inhibitor or finerenone might help you.
- Write down your numbers. Track them. Bring them to every visit.
Diabetic kidney disease doesn’t happen overnight. But it doesn’t stop either-unless you act. The science is clear. The tools exist. The only thing missing is urgency.
Can albuminuria be reversed?
Yes, in many cases. Studies show that with tight blood sugar control, blood pressure management, and medications like ACE inhibitors or SGLT2 inhibitors, albuminuria can drop significantly-even return to normal levels. The earlier you start, the better your chances. Some patients with moderately increased albuminuria (30-300 mg/g) see their levels fall below 30 mg/g within 6-12 months of starting full treatment.
Do I need to collect urine for 24 hours to test for albuminuria?
No. The standard test is a spot urine sample measured as UACR (urine albumin-to-creatinine ratio). It’s just as accurate as a 24-hour collection and much easier. Timed collections (like overnight) are only used in research or if spot results are unclear. Most clinics use spot tests because they’re practical and reliable.
If I have albuminuria, do I need to see a kidney specialist?
Not always-but you should if your UACR is over 300 mg/g, your eGFR is below 60, or your condition isn’t improving despite treatment. Primary care providers can manage early-stage DKD, but nephrologists offer advanced tools, faster medication titration, and access to newer drugs like finerenone. If you’ve been told to "wait and see" for more than a year, ask for a referral.
Can I stop taking my kidney-protective meds if my albuminuria improves?
No. Even if your UACR drops to normal, you still need to keep taking your ACE inhibitors, ARBs, SGLT2 inhibitors, or finerenone. These drugs don’t just mask symptoms-they change the underlying disease process. Stopping them can cause albuminuria to return and your kidney damage to resume. Think of them like insulin for your kidneys: you need them to stay protected.
Are there natural ways to reduce albuminuria?
Diet and lifestyle help-but they’re not enough on their own. Reducing salt, losing weight, quitting smoking, and avoiding NSAIDs (like ibuprofen) can lower albuminuria slightly. But the only proven ways to significantly reduce it are medications: RAAS blockers, SGLT2 inhibitors, and finerenone. Lifestyle changes support these drugs, but they don’t replace them.
How often should I get my UACR tested?
If you have diabetes and no albuminuria, get tested once a year. If you’ve been diagnosed with albuminuria, get tested every 3-6 months until your levels stabilize. After that, annual testing is usually enough-unless your doctor changes your meds or your numbers start rising again. Always test after any illness, infection, or hospital stay, since those can cause temporary spikes.






Deepak Mishra
OMG!!! This is LIFE-CHANGING!!! I had microalbuminuria last year and thought it was just a typo on my lab report… turned out I was at 140 mg/g!!! Now I’m on SGLT2 inhibitors, lost 32 lbs, and my UACR is down to 22!!! GOD BLESS SCIENCE!!! 😭🙏🔥
Teresa Smith
The data is unequivocal: early intervention through glycemic and blood pressure control alters the natural history of diabetic kidney disease. The metabolic memory phenomenon observed in DCCT/EDIC underscores that transient but rigorous control yields durable protection. This is not merely preventive medicine-it is restorative physiology. Clinicians must prioritize UACR screening as a non-negotiable biomarker, not an optional add-on. The cost of inaction is measured in dialysis, transplantation, and premature mortality.
ZAK SCHADER
So we’re supposed to believe that some fancy lab test from a government-funded study is gonna save us? Meanwhile, our hospitals are full of people on insulin pumps and metformin, and their kidneys still fail. This is just another way for Big Pharma to sell more drugs. We need less testing and more real food-no more processed carbs, no more insulin dependence. America’s diabetes crisis is a political failure, not a medical one.
Danish dan iwan Adventure
Albuminuria >30 mg/g = glomerular endothelial dysfunction. HbA1c >7% = hyperglycemic toxicity. BP >130/80 = RAAS overactivation. Three pillars. Fail one, fail all. No ambiguity. No exceptions. Test annually. Treat aggressively. No excuses.
Ankit Right-hand for this but 2 qty HK 21
Typical Western medical dogma. In India, we’ve been managing this with Ayurveda for centuries-turmeric, fenugreek, bitter gourd. No drugs, no labs, just wisdom. Now you want us to pay $200 for a urine test? Pathetic. Your system is broken. You’re diagnosing symptoms, not curing root causes. Your hospitals are profit centers, not healing spaces.
Oyejobi Olufemi
You think this is about kidneys? No. This is about control. The pharmaceutical-industrial complex needs you dependent. They invented "microalbuminuria" to create a new disease category so they could sell you drugs for 40 years. The ADA? Owned by Big Pharma. The SPRINT trial? Funded by Novo Nordisk. The 7% HbA1c target? Arbitrary. Your blood sugar was fine before they told you it wasn’t. They don’t want you cured-they want you compliant. Wake up.
Rachel Wusowicz
I read this and started crying. Not because I’m scared-but because I realized I’ve been ignoring my body for 12 years. I thought "I feel fine" meant I was fine. I didn’t know my kidneys were screaming. I got my UACR tested last week-112 mg/g. I’m terrified. But I’m also… determined. I’m going to the dietitian tomorrow. I’m buying a glucose monitor. I’m quitting soda. I’m not waiting for the next test. I’m not waiting for the next warning. I’m done waiting. I’m done pretending.
Dan Angles
Thank you for sharing this nuanced perspective. The data is clear, but human behavior is complex. We must recognize that structural barriers-lack of access, insurance limitations, provider bias, and health literacy gaps-prevent even the most motivated patients from adhering to guidelines. While tight control is ideal, we must also advocate for systemic change: universal screening protocols, automated EHR alerts, community health worker programs, and equitable access to SGLT2 inhibitors and GLP-1 RAs. Prevention is not just clinical-it is ethical.