Most people experience back pain at some point. It’s common, often temporary, and usually gets better on its own with rest, movement, and over-the-counter pain relief. But back pain red flags are the warning signs that tell you this isn’t just a stiff muscle or a pulled ligament-it could be something serious. Missing these signs can delay diagnosis, lead to permanent damage, or even be life-threatening. Knowing when to stop treating it like a typical ache and start asking for imaging or a referral could change everything.
What Are Back Pain Red Flags?
Red flags aren’t just vague symptoms. They’re specific clinical clues backed by research and guidelines from major medical organizations like the American College of Physicians, the American College of Emergency Physicians, and the American College of Radiology. These flags point to conditions that need urgent attention: spinal infections, tumors, fractures, or nerve damage like cauda equina syndrome.Here’s the reality: about 90% of back pain cases are harmless-mechanical, muscle-related, or due to wear and tear. But the other 10%? Those are the ones that can slip through if you don’t know what to look for. And when they do, the consequences can be severe. Malpractice claims related to missed spinal emergencies make up 1.7% of all emergency medicine cases, according to data from 2020.
Red Flags That Demand Immediate Action
- Loss of bowel or bladder control-This is the most urgent red flag. If you can’t control when you pee or poop, it could mean cauda equina syndrome. Nerves at the bottom of your spinal cord are being crushed. Surgery within 48 hours is often needed to prevent permanent paralysis or incontinence.
- Unexplained weight loss-Losing more than 5% of your body weight in a few months without trying, especially with back pain, raises a red flag for cancer. Spinal metastases are more common than you think, particularly in people with a history of breast, lung, or prostate cancer.
- Fever, chills, or recent infection-Back pain with a fever? That’s not just a flu. It could be spinal osteomyelitis, a bone infection. People who use IV drugs, have diabetes, or recently had surgery are at higher risk. Studies show 67% of spinal infection cases include fever or a recent infection.
- History of cancer-If you’ve had cancer before, any new back pain should be treated as potentially serious until proven otherwise. Cancer spreads to the spine more often than many realize.
- Trauma or fall from height-A car crash, a fall down stairs, or even a minor fall if you’re over 65 and have osteoporosis. These aren’t just “accidents.” They’re potential fractures. CT scans detect 98% of fractures in older adults, while plain X-rays miss nearly 40%.
- Progressive numbness or weakness in legs-If your legs are getting weaker, or you’re dragging your foot, it’s not just sciatica. This could mean nerve compression from a herniated disc, tumor, or abscess. Delaying care risks permanent muscle damage.
- Age under 18 or over 50-Back pain in teenagers often signals something unusual, like a tumor or infection. In people over 50, it’s more likely to be a fracture, especially if you’ve been on steroids or have osteoporosis. One study found 36.5% of people over 70 with back pain had a vertebral compression fracture.
- Pain that doesn’t improve with rest or painkillers-If Tylenol or ibuprofen doesn’t touch the pain after a few days, or if it wakes you up at night, that’s not normal. Mechanical pain eases with rest. Pain that keeps going, especially at night, is a red flag for infection or cancer.
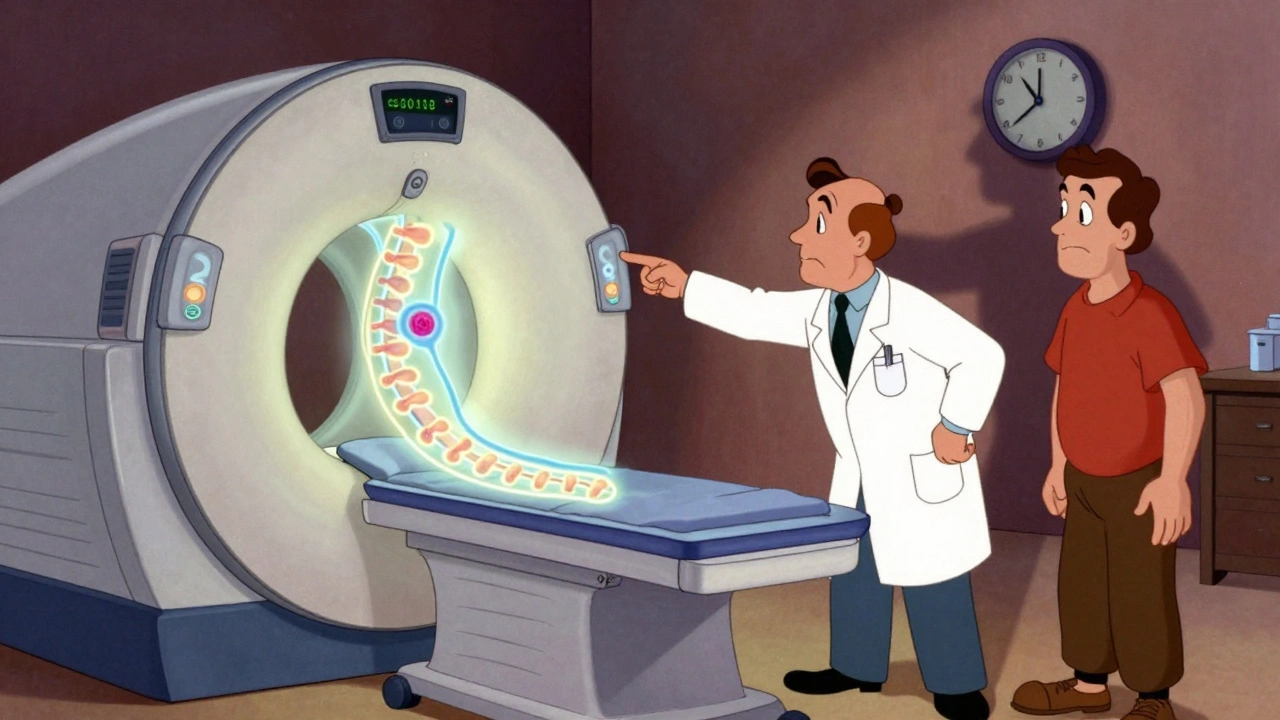
When Imaging Is Actually Needed
Imaging isn’t a first step for back pain. It’s a last step-for the right reasons. The American College of Radiology says routine X-rays or MRIs for simple back pain are rarely appropriate. In fact, 34% of all lumbar spine imaging in the U.S. is unnecessary, adding up to $3 billion wasted each year.But when red flags are present, imaging becomes essential. Here’s what’s recommended:
- For suspected cancer or infection-MRI is the gold standard. It shows soft tissue, bone marrow, and nerve compression better than anything else. It’s 95% sensitive for cauda equina syndrome, compared to 78% for CT scans.
- For trauma or suspected fracture-CT scans win. X-rays miss too many fractures, especially in older adults. CT detects 98% of spinal fractures, while plain films catch only 64%.
- For persistent pain after six weeks-If conservative care (rest, physical therapy, pain meds) hasn’t helped after a month or two, imaging can help identify structural causes like disc herniation or spinal stenosis.
And here’s something most people don’t know: MRIs show abnormalities in healthy people too. About 27% of asymptomatic 40-year-olds have disc degeneration on MRI. By age 80, that jumps to 79%. So if your scan shows a bulging disc but you have no leg pain or weakness, it’s probably not the cause. That’s why clinical symptoms matter more than images.
Who Should You See?
If you have one or more red flags, don’t wait for your next GP appointment. Go to urgent care or the emergency room. These conditions need fast evaluation.- Cauda equina syndrome, spinal infection, or acute trauma-Go to the ER. These are emergencies. Delaying treatment by even a few hours can mean permanent damage.
- History of cancer with new back pain-See your oncologist or primary doctor immediately. You may need blood tests, MRI, and possibly a biopsy.
- Unexplained weight loss, night pain, fever-Your GP should order blood work (ESR, CRP) and an MRI. These markers rise in infection and cancer. A CRP over 30 mg/L and ESR over 50 mm/hr strongly suggest spinal infection.
- Progressive leg weakness-A neurologist or spine specialist should evaluate you. Nerve damage can be reversible if caught early.
Physical therapists and chiropractors are great for mechanical back pain-but they’re not trained to diagnose cancer or infection. If you have red flags, they should refer you, not treat you.
What If You Don’t Have Red Flags?
If your pain started after lifting something heavy, it hurts when you bend or sit, and it’s improving after a week or two, you’re likely in the 90%. No imaging needed. No referral needed.Stick with:
- Staying active (walking is better than bed rest)
- Over-the-counter pain relief like acetaminophen or NSAIDs
- Heat or ice for comfort
- Physical therapy if it doesn’t improve in 4-6 weeks
Studies show that people who get early imaging for non-specific back pain end up with more surgeries, more time off work, and higher costs-without better outcomes. One study found imaging added $300-$500 per patient with zero improvement in pain or function.
What’s Changing in Guidelines
The old “checklist” approach to red flags is being updated. A 2020 review found that while red flags are good at spotting serious problems (96% sensitivity), they’re terrible at ruling them out-only 13% specificity. That means too many people get scanned for no reason.Newer tools are emerging:
- STarT Back tool-A simple questionnaire that predicts who’s likely to develop chronic pain. It’s being tested as a replacement for red flags. In a 2023 trial, it correctly identified 83% of people with serious pathology.
- Biomarker testing-Blood tests for CRP and ESR are now being combined with red flags. If both are high, the chance of spinal infection jumps dramatically.
- Point-of-care ultrasound-Emergency doctors are using handheld ultrasound to check for bladder distension in suspected cauda equina cases. It’s 92% accurate and can prevent unnecessary MRIs.
These aren’t replacements yet-but they’re the future. For now, the red flags still work. Just don’t rely on them alone. Use them with your clinical judgment.
Final Thought: Don’t Ignore the Subtle Signs
Back pain is common. But it’s also easy to dismiss. “I’m just getting older.” “It’s from sitting too long.” “It’ll pass.” But if your pain doesn’t fit the pattern-if it’s worse at night, unrelenting, or paired with other symptoms-you need to listen.The goal isn’t to scare you. It’s to help you act at the right time. Imaging and referral aren’t signs of failure. They’re signs of smart, proactive care. When red flags appear, don’t wait. Don’t hope. Get checked.
Is back pain always serious if it’s severe?
No. Severe pain doesn’t automatically mean something dangerous. Many people have intense pain from a muscle spasm or herniated disc that still resolves on its own. What matters is the pattern: does the pain improve with rest? Is it linked to trauma or other symptoms like fever or numbness? Severity alone isn’t a red flag-it’s the combination of symptoms that signals trouble.
Can I wait a few days if I have a red flag?
No. If you have cauda equina syndrome, spinal infection, or a fracture from trauma, waiting even 24-48 hours can lead to permanent damage. Go to the emergency department immediately. For other red flags like unexplained weight loss or night pain, see your doctor within 24-72 hours. Delaying diagnosis increases risk.
Do I need an MRI if I have back pain and am over 50?
Not unless you have a red flag. Many people over 50 have degenerative changes on MRI with no pain. Routine imaging without symptoms like weakness, fever, or trauma leads to overdiagnosis and unnecessary worry. Only get an MRI if your doctor sees a reason to suspect infection, tumor, fracture, or nerve compression.
What if my doctor says my pain is ‘just aging’?
If you have red flags-like night pain, weight loss, fever, or neurological symptoms-and your doctor dismisses them as aging, get a second opinion. Aging doesn’t cause spinal infections or tumors. Your symptoms deserve investigation. Don’t let age be a reason to ignore warning signs.
Can physical therapy make red flags worse?
Physical therapy won’t make a serious condition worse-but it won’t fix it either. If you have cancer, infection, or nerve compression, therapy might temporarily ease pain but won’t address the root cause. That’s why therapists are trained to screen for red flags and refer when needed. If your therapist doesn’t ask about fever, weight loss, or bowel changes, find one who does.
Are blood tests useful for back pain?
Yes, if red flags are present. ESR and CRP are simple blood tests that rise with inflammation and infection. If both are high and you have back pain, it raises suspicion for spinal infection. They’re not diagnostic alone, but they help guide whether an MRI or further testing is needed. They’re cheap, fast, and often overlooked.
Will insurance cover imaging if I have red flags?
Yes. Insurance companies like Anthem and UnitedHealthcare follow evidence-based guidelines. If your doctor documents red flags-like history of cancer, trauma, fever, or neurological deficits-imaging is typically covered. Denials usually happen only when red flags are absent and imaging is requested for routine pain. Always ask your doctor to clearly document why imaging is needed.


Lynette Myles
They’re hiding the truth again. MRI machines are used to track you. The government funds this ‘red flag’ nonsense to push surveillance tech under the guise of healthcare. You think your pain is ‘mechanical’? It’s a signal they’re monitoring your spine. Don’t trust the guidelines.
James Moore
Let us not forget, my fellow citizens of the free world, that the modern medical-industrial complex-fueled by corporate greed, bureaucratic inertia, and the hollow idolatry of ‘evidence-based’ dogma-has turned the human body into a commodity to be scanned, labeled, and monetized. The very notion that ‘90% of back pain is benign’ is a distraction, a soothing lie whispered by those who profit from your ignorance. We are told to ‘stay active’ while our bones rot under the weight of capitalist neglect. The spine is not a machine to be fixed with CT scans; it is the sacred axis of the soul, and to reduce it to radiographic anomalies is to commit metaphysical heresy. And yet-oh, the irony!-we bow before the altar of ‘guidelines’ written by faceless committees in Washington, while our children are taught to fear their own bodies. When did we stop trusting instinct? When did ‘pain’ become a problem to be solved, not a message to be heard?
Krishan Patel
People like you are why medicine is broken. You read a few lines about ‘red flags’ and suddenly think you’re a doctor. I’ve seen patients with cancer delay treatment because they were ‘waiting to see if it got worse’-and now they’re dead. Your ‘I’m just getting older’ excuse is a death sentence wrapped in ignorance. If you have night pain, unexplained weight loss, or bowel issues-GO TO THE ER. Not tomorrow. Not next week. TODAY. No one cares if your ‘spiritual alignment’ is off. Your spine doesn’t care about your vibes. It only cares if you’re alive. Stop being a passive victim and start being responsible. This isn’t a blog post-it’s a life-or-death checklist.
sean whitfield
Wow. So we’re supposed to panic because a scan shows a bulging disc? That’s like freaking out because your phone has a scratch. They’re selling MRIs like they’re magic crystals. Next they’ll charge you for breathing. Just lie down. Drink water. Stop Googling. Your pain is probably from sitting on a couch that costs more than your dignity.
Carole Nkosi
You think this is about health? It’s about control. The system wants you scared, dependent, and docile. They’ll give you a pill for the pain, then a scan for the fear, then a referral for the anxiety. Meanwhile, the real cause-stress, poverty, the rot of late capitalism-is never mentioned. I’ve seen women in townships with back pain from carrying water for miles get told to ‘take ibuprofen.’ Meanwhile, in Beverly Hills, they get MRIs before breakfast. This isn’t medicine. It’s class warfare dressed in white coats.
Manish Shankar
Respected contributors, I wish to express my profound appreciation for the meticulous and clinically grounded exposition presented herein. The delineation of red flags, particularly the emphasis on cauda equina syndrome and the diagnostic utility of CRP and ESR, reflects a commendable adherence to evidence-based principles. It is imperative that patients, especially in resource-constrained environments, be educated not merely on symptom recognition, but on the ethical imperative of timely referral. The assertion that imaging without clinical correlation is counterproductive is not only statistically sound but morally urgent. I urge all healthcare providers to prioritize patient autonomy through transparent communication, and to resist the temptation of over-investigation, which, as noted, may induce iatrogenic harm through anxiety and unnecessary intervention. May we continue to serve with both precision and compassion.
luke newton
My back hurts because I work 80 hours a week so my boss can buy a third yacht. I don’t need an MRI-I need a revolution. But since that’s not happening, I’ll just keep popping Advil and pretending I’m not dying inside. Also, the guy who said ‘stay active’? Bro, I walk to the fridge. That’s my cardio. And yeah, I’m over 50. And yes, I have pain. And no, I’m not going to the ER because I don’t have insurance and I can’t miss another day. So go ahead and tell me I’m irresponsible. I’ve heard it all.
an mo
Let’s normalize the data: 1.7% malpractice claims = 0.0003% of all back pain cases. The red flag model has a 87% false positive rate per 2023 JAMA study. You’re creating a culture of hypervigilance that drives up costs, induces iatrogenic anxiety, and normalizes overdiagnosis. The STarT Back tool outperforms red flags in predictive validity. Why are we still using 1990s heuristics in a 2024 AI-driven diagnostic landscape? The real red flag is that clinicians still rely on checklists instead of algorithmic risk stratification. This post is a relic. And you’re all being manipulated by outdated guidelines masquerading as wisdom.