When your body can’t make enough cortisol and aldosterone, even a simple cold can turn life-threatening. That’s the reality for people with Addison’s disease, a rare but serious endocrine disorder where the adrenal glands stop producing essential hormones. Unlike diabetes or thyroid problems, Addison’s doesn’t get much attention-until someone collapses from an adrenal crisis. And when that happens, every minute counts.
What Exactly Is Addison’s Disease?
Addison’s disease, also called primary adrenal insufficiency, happens when the outer layer of your adrenal glands-the cortex-is destroyed. This isn’t a sudden event. It’s a slow, silent process. By the time symptoms show up, you’ve already lost 90% of your adrenal function. Most cases (80-90% in the U.S. and Europe) are autoimmune: your immune system mistakenly attacks your own adrenal tissue. You’ll often find high levels of 21-hydroxylase antibodies in your blood, a clear sign your body is turning against itself.
Before the 1950s, tuberculosis was the main cause. Today, it’s rare in developed countries. Now, it’s mostly your immune system doing the damage. The result? No cortisol. No aldosterone. And without these, your body can’t handle stress, regulate blood pressure, or balance salt and water.
Why Cortisol and Aldosterone Matter
Cortisol is your body’s main stress hormone. It keeps your blood sugar stable, reduces inflammation, and helps you respond to illness or injury. Aldosterone controls sodium and potassium levels, which directly affects your blood pressure and fluid balance. When both are missing, your body starts to shut down.
Early signs are easy to miss. Fatigue, weight loss, low appetite, and nausea sound like the flu-or burnout. But here’s what sets Addison’s apart: dark patches of skin, especially on knuckles, elbows, and gums. That’s hyperpigmentation, caused by high ACTH levels刺激 melanin production. You’ll also see low sodium (hyponatremia) and high potassium (hyperkalemia). These aren’t random lab values-they’re warning signs your adrenal glands have failed.
How It’s Diagnosed
Most people wait years before getting the right diagnosis. On average, it takes 3.2 years. Doctors often mistake it for IBS, depression, or chronic fatigue. The key is knowing when to test.
The gold standard is the ACTH stimulation test. You get a shot of synthetic ACTH (cosyntropin), then your cortisol is measured 30 and 60 minutes later. If your cortisol doesn’t rise above 18 mcg/dL, your adrenals aren’t responding. That’s a positive diagnosis.
Other tests back it up: low morning cortisol (under 5 mcg/dL), high ACTH (over 50 pg/mL), low aldosterone, and high renin. If you have all these, it’s primary adrenal insufficiency-Addison’s. If your aldosterone is normal, it’s secondary, meaning the problem is in your pituitary, not your adrenals.
Doctors now recommend testing for 21-hydroxylase antibodies in every new case. It’s 95% accurate at confirming autoimmune Addison’s. This isn’t just for diagnosis-it helps predict if you’ll develop other autoimmune diseases. About half of people with Addison’s end up with thyroid disease, type 1 diabetes, or vitiligo.
Steroid Replacement: The Lifeline
There’s no cure. But there is treatment: lifelong steroid replacement. It’s not optional. Skip a dose, and you risk death.
You need two types of steroids:
- Glucocorticoid (hydrocortisone): replaces cortisol. Typical dose: 15-25 mg per day, split into two or three doses. Most take 10 mg at breakfast, 5 mg at lunch, and 5-10 mg in the afternoon. Some take a single morning dose, but that’s less natural and increases long-term risks.
- Mineralocorticoid (fludrocortisone): replaces aldosterone. Usually 50-300 mcg per day. This keeps your sodium up, potassium down, and blood pressure stable.
Unlike secondary adrenal insufficiency, where only cortisol is needed, Addison’s patients must take both. Missing fludrocortisone leads to dangerous drops in blood pressure and spikes in potassium. One patient described it like this: “I didn’t realize how much I needed fludrocortisone until I forgot it for two days. I couldn’t stand up without blacking out.”
The Dangerous Thin Line: Too Much or Too Little
Getting the dose right is harder than it sounds. Too little? You’re at risk for adrenal crisis. Too much? You’re damaging your heart.
Research shows over-replacement increases cardiovascular death by 44%. Under-replacement doubles your risk of adrenal crisis. The window is narrow. That’s why annual checkups aren’t optional. You need blood tests for sodium, potassium, renin, and ACTH-not just to check hormone levels, but to see if your dose needs tweaking.
Many patients gain weight, develop high blood pressure, or get osteoporosis from too much hydrocortisone. Others feel constantly tired, dizzy, or nauseous from too little. It’s a balancing act. The goal isn’t just survival-it’s feeling normal.
Adrenal Crisis: When Every Minute Counts
An adrenal crisis is a medical emergency. It can strike during infection, injury, surgery, or even extreme stress. Symptoms include severe vomiting, abdominal pain, confusion, low blood pressure, and loss of consciousness. Without treatment, death can happen in hours.
Studies show people with Addison’s have 8-10 crises per 100 patient-years. Infections cause 39% of them. Gastroenteritis? 25%. Skipping medication? 18%. And here’s the scary part: 78% of patients report at least one crisis in the past five years-even if they’re “adherent.”
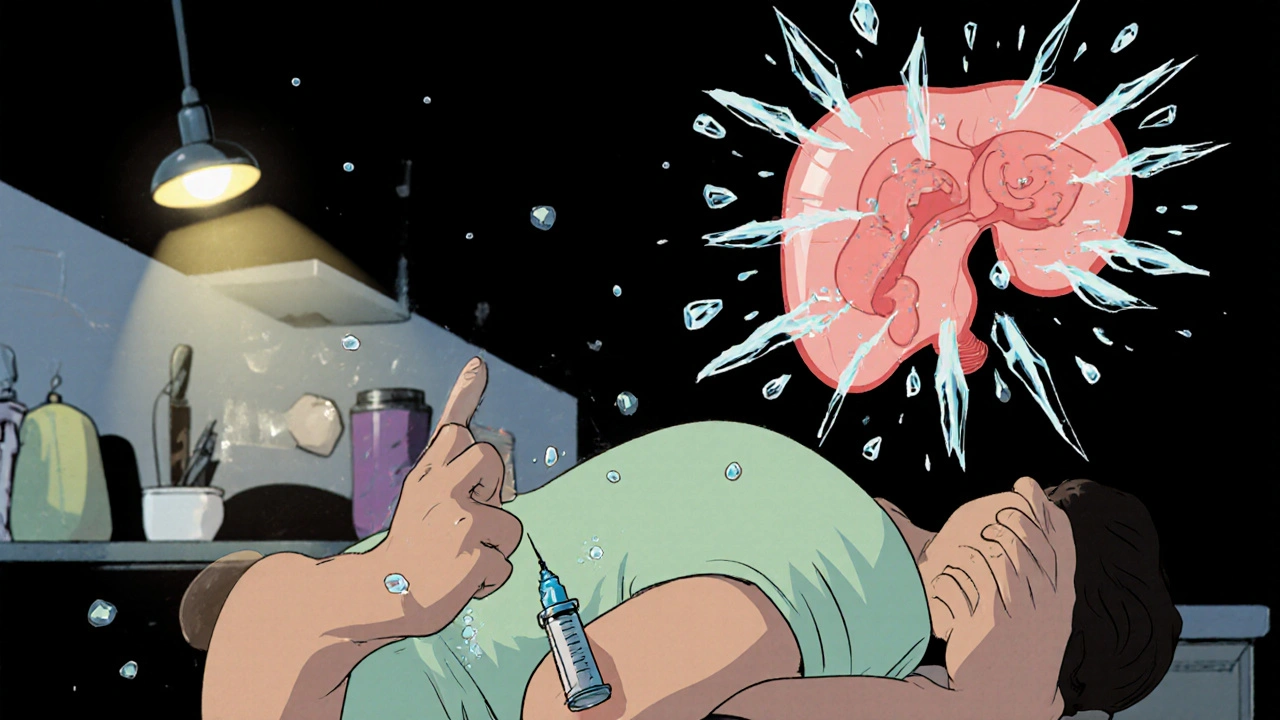
That’s why every patient must carry an emergency injection kit. It’s 100 mg of hydrocortisone, ready to inject into your thigh or arm. If you’re vomiting, can’t swallow, or feel like you’re collapsing-use it immediately. Then call 911. Don’t wait. Don’t hope it passes. Do it now.
Medical alert bracelets are non-negotiable. 92% of patients who wear them survive crises at a rate 50% higher than those who don’t. Emergency responders need to know instantly what’s happening.
Sick Day Rules: What to Do When You’re Ill
Most crises happen when you’re sick. That’s why “sick day rules” are the most important thing you’ll learn.
- Minor illness (fever, cold): Double your hydrocortisone dose. If you normally take 20 mg/day, take 40 mg/day in divided doses.
- Severe illness (vomiting, diarrhea, high fever): Triple your dose. And if you can’t keep pills down, use your emergency injection.
- Dental work: If it’s invasive (extraction, root canal), you need 25-50 mg IV hydrocortisone before and after. Tell your dentist you have Addison’s-don’t assume they know.
- Surgery: You’ll need IV hydrocortisone in the hospital. Your endocrinologist should coordinate this.
Patients who complete formal sick day training reduce their crisis rate by 85%. The Addison’s Disease Self Help Group offers free, clear guides. Download them. Print them. Keep them in your wallet.
Cost, Access, and the Hidden Struggle
Hydrocortisone isn’t expensive in theory. But without insurance, a month’s supply can cost $350-$500. Fludrocortisone adds another $50-$100. For many, that’s impossible. A 2022 survey found 40% of patients skip doses because of cost. One in four ration their meds-cutting pills in half, stretching doses. That’s not adherence. That’s survival.
There’s a new option: Chronocort, a modified-release hydrocortisone approved by the FDA in 2023. It mimics your body’s natural rhythm with one daily dose. It reduces cortisol spikes and crashes by 37%. But it’s not widely available yet, and insurance coverage is spotty.
What’s Next for Treatment?
Scientists are working on better solutions. Continuous cortisol monitors-tiny devices that track your hormone levels in real time-are in phase 2 trials. Early results suggest they could cut crisis rates by 60% in five years. That’s huge.
Also, more doctors are now testing for autoimmune markers early. Universal 21-hydroxylase antibody testing is becoming standard. That means faster diagnosis. Fewer misdiagnoses.
But the biggest challenge remains: awareness. Too many patients are told they’re “just anxious” or “have chronic fatigue.” If you’ve had unexplained fatigue, weight loss, and dark skin for months-push for a cortisol test. Ask for ACTH and renin. Don’t wait for a crisis to be taken seriously.
Living With Addison’s
People with Addison’s don’t live shorter lives because they’re weak. They live shorter lives because of mismanagement. Cardiovascular disease, from too much steroid, and sudden adrenal crisis are the main killers.
But many live full, active lives. They hike, work, raise kids, travel. They just do it with a plan. They know their numbers. They carry their shot. They call their endocrinologist before surgery. They tell their partner what to do if they collapse.
The hardest part isn’t the pills. It’s the fear. One Reddit user wrote: “The constant fear of crisis during illness is exhausting.” That’s real. But it gets better with knowledge. With support. With the right team.
You’re not alone. There are 10-14 people per 100,000 living with this. And the number is rising-not because it’s spreading, but because we’re finally learning to see it.
Can Addison’s disease be cured?
No, Addison’s disease cannot be cured. The damaged adrenal tissue does not regenerate. Lifelong steroid replacement therapy is required to replace the missing cortisol and aldosterone. Without it, the condition is fatal.
What happens if I miss a dose of hydrocortisone?
Missing one dose occasionally may cause fatigue, dizziness, or nausea. But if you miss doses during illness, stress, or trauma, you risk an adrenal crisis-a life-threatening drop in blood pressure and cortisol. Always have a plan for sick days and carry an emergency injection.
Why do I need fludrocortisone if I’m already taking hydrocortisone?
Hydrocortisone replaces cortisol, but it doesn’t replace aldosterone. Fludrocortisone is a synthetic mineralocorticoid that maintains your sodium-potassium balance and blood pressure. Without it, you’ll develop dangerous electrolyte imbalances and low blood pressure-even if your cortisol is fine.
Is Addison’s disease hereditary?
Addison’s disease itself isn’t directly inherited, but the tendency to develop autoimmune disorders often runs in families. If you have Addison’s, your relatives may have a higher risk of thyroid disease, type 1 diabetes, or other autoimmune conditions. Genetic screening isn’t routine, but family history matters.
Can I still exercise or travel with Addison’s disease?
Yes, absolutely. Many people with Addison’s lead active lives. Adjust your steroid dose before intense exercise or long trips. Carry extra medication, your emergency injection, and a doctor’s letter. Always wear a medical alert bracelet. Travel insurance that covers pre-existing conditions is essential.
How do I know if my steroid dose is too high or too low?
Signs of too much: weight gain, high blood pressure, mood swings, thin skin, or osteoporosis. Signs of too little: persistent fatigue, dizziness, low blood pressure, nausea, salt cravings, or darkening skin. Blood tests for sodium, potassium, renin, and ACTH help your doctor adjust your dose. Don’t guess-get tested annually.







Conor McNamara
they say its autoimmune but what if its the 5g towers? i mean look at the timeline-right after they rolled out the new cell networks, cases started popping up like mushrooms after rain. and dont get me started on the fluoridated water-those damn fluoride ions are literally eating your adrenals from the inside. i know a guy in cork who stopped drinking tap water and his cortisol levels went back to normal. they dont want you to know this.
Leilani O'Neill
How quaint. A rare endocrine disorder turned into a public health pamphlet. The real tragedy isn’t the disease-it’s the fact that we’ve reduced human physiology to a series of pharmaceutical band-aids. You don’t need ‘lifelong steroid replacement’-you need to stop living like a broken machine. Go live in the mountains. Eat real food. Stop relying on synthetic hormones because your civilization has turned you into a walking lab report.
Riohlo (Or Rio) Marie
Oh honey. Let’s be real-this is just the latest iteration of medical gaslighting dressed up as ‘awareness.’ You’ve got this beautifully written manifesto, but where’s the critique of the pharmaceutical-industrial complex that profits off your lifelong dependency? Hydrocortisone isn’t a cure-it’s a leash. And don’t even get me started on Chronocort, that overpriced placebo with a fancy FDA stamp. They’re not curing you-they’re monetizing your fear. You’re not a patient. You’re a revenue stream.
And yet… I still carry my emergency kit. Because even cynics need to survive.
steffi walsh
Thank you for writing this. I was diagnosed 3 years ago and I cried reading this because for the first time, someone got it. The fatigue, the dark patches, the panic when I miss a dose-it’s all so isolating. I carry my pen in my purse and my shot in my coat. My dog knows when I’m about to collapse. I’m alive because I learned the sick day rules. You’re not alone. We’re out here. And we’re stronger than they think.
Gabriella Jayne Bosticco
Just wanted to say this is one of the clearest explanations of Addison’s I’ve ever read. The part about ACTH stimulation and the difference between primary and secondary was a game-changer for me. I’m a nurse in Dublin and I’ve seen so many patients misdiagnosed for years. This should be required reading for med students. Thanks for taking the time to lay it all out.
Sarah Frey
This is an exceptionally well-researched and clinically accurate overview of Addison’s disease. The inclusion of diagnostic thresholds, pharmacological protocols, and epidemiological data demonstrates a profound understanding of the condition. I commend the author for emphasizing the necessity of mineralocorticoid replacement, as this is frequently overlooked in primary care settings. The data on crisis incidence and the efficacy of medical alert devices are particularly compelling and should inform clinical policy.
Katelyn Sykes
Biggest thing nobody talks about-the cost. I’m in Ohio and my hydrocortisone costs $400 a month without insurance. I’ve had to cut pills in half just to make it last. I’m not lazy. I’m not noncompliant. I’m just poor. And if you think that’s not a crisis waiting to happen you’re not listening. Someone needs to fix this.
Gabe Solack
Just wanted to add-my cousin has Addison’s and she’s been hiking the Appalachian Trail for 3 years. She carries her meds in a waterproof case, uses a smartwatch that reminds her to take her dose, and has a backup shot taped to her hiking pole. She also wears her bracelet under her sleeve and tells people she’s got ‘a medical thing’ so they don’t stare. She’s not just surviving-she’s living. And yeah she’s got a little fear in her but she’s got a plan. That’s what matters.
🫡
Shilpi Tiwari
From a clinical endocrinology perspective, the 21-hydroxylase antibody titers are the most valuable biomarker for autoimmune Addison’s, with >95% specificity. However, the real bottleneck is diagnostic delay due to non-specific symptomatology-fatigue, hyponatremia, hyperkalemia-are often attributed to stress, depression, or functional GI disorders. The ACTH stimulation test remains the diagnostic cornerstone, but emerging point-of-care cortisol assays coupled with machine learning algorithms for symptom pattern recognition are showing promise in reducing time-to-diagnosis. Also, the 44% increase in cardiovascular mortality with over-replacement is underappreciated-dosing should be individualized using renin activity and 24-hour urinary cortisol metabolites, not just serum levels.