RAAS Inhibitors: How They Work and What You Need to Know
When your body’s RAAS inhibitors, a class of drugs that block the renin-angiotensin-aldosterone system to lower blood pressure and protect organs. Also known as renin-angiotensin system blockers, these medications are among the most prescribed for people with high blood pressure, heart failure, or diabetic kidney damage. They don’t just reduce numbers on a monitor—they slow down damage to your heart and kidneys by calming a system that, when overactive, squeezes blood vessels too hard and holds onto too much salt and water.
There are a few main types you’ll see in practice. Angiotensin-converting enzyme inhibitors, drugs like lisinopril and enalapril that stop the body from making a hormone that tightens blood vessels, are often the first choice. Then there’s angiotensin II receptor blockers, medications like losartan and valsartan that block the hormone’s effect at the receptor level, which work similarly but cause fewer coughs. And then you’ve got combinations—like Combipres, a pill that pairs clonidine with chlorthalidone to hit blood pressure from two angles—used when one drug isn’t enough. These aren’t just random pills; they’re tools that target the same system in different ways, and doctors pick based on your body’s response.
RAAS inhibitors often show up alongside other treatments you might not realize are connected. For example, amiloride, a potassium-sparing diuretic that prevents the body from losing too much potassium while flushing out excess fluid, is sometimes used with RAAS blockers because they both help manage fluid balance without dropping potassium too low. That’s why you’ll see posts about fluid retention and diuretics for kidney disease here—these aren’t separate topics. They’re parts of the same puzzle. People with chronic kidney disease, heart failure, or even just stubborn high blood pressure often end up on a mix of these drugs because they work better together than alone.
What’s interesting is how often these drugs show up in real-life cases. Someone with diabetes might be on an ACE inhibitor to protect their kidneys, even if their blood pressure is normal. Someone with edema from kidney trouble might get a diuretic along with an ARB. And if they’re still struggling with swelling, a doctor might add a potassium-sparing agent like amiloride to keep things balanced. It’s not magic—it’s science layered on top of science, tailored to your body’s signals.
You’ll find posts here that break down exactly how these drugs compare, what side effects to watch for, and why some people respond better to one type than another. Whether you’re trying to understand why your doctor switched your meds, or you’re just curious how your blood pressure pills actually work, the articles below give you the real details—not just textbook definitions. No fluff. Just what you need to know to make sense of your treatment and ask better questions.
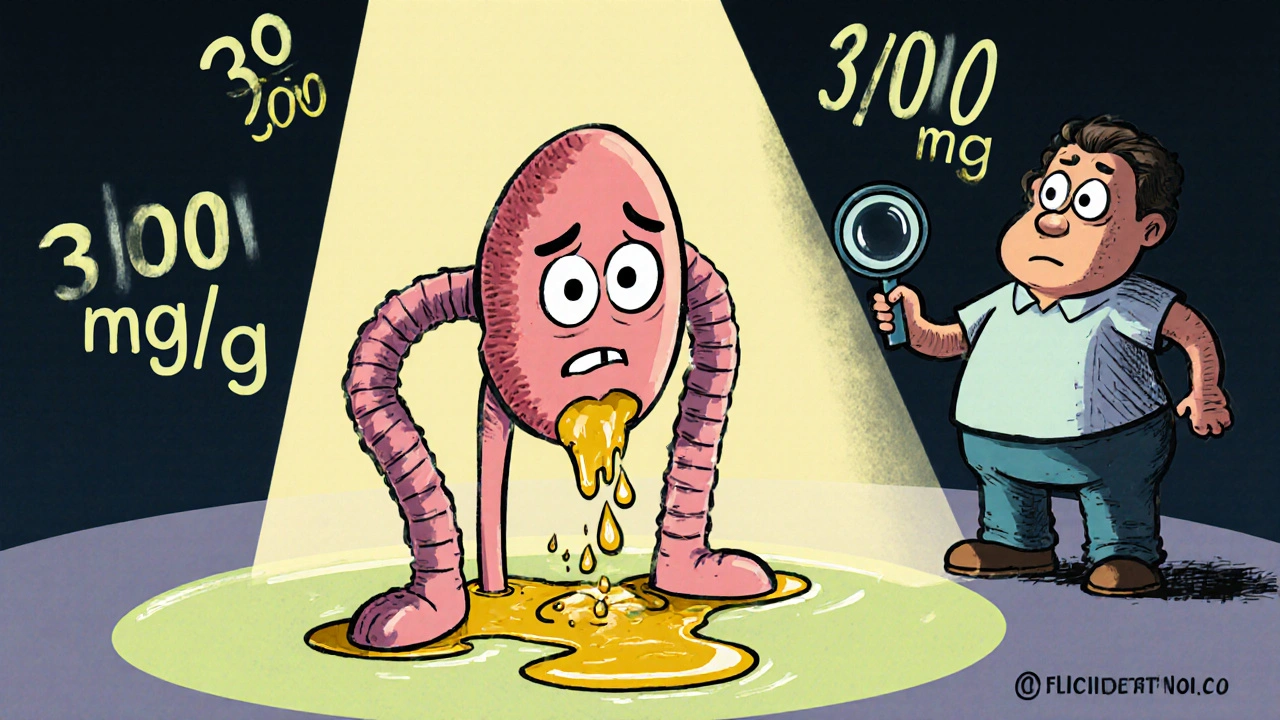
Diabetic Kidney Disease: How Early Albuminuria Signals Risk and Why Tight Control Saves Kidneys
Diabetic kidney disease often starts with silent albuminuria. Early detection and tight control of blood sugar, blood pressure, and targeted medications can prevent kidney failure. Learn how to act before it's too late.