Patient Exposure Calculator
Every year, dozens of medications are pulled from store shelves and doctor’s offices-not because they’re outdated, but because they’re unsafe or simply don’t work. These aren’t minor glitches. They’re life-or-death decisions made by regulators, manufacturers, and sometimes, too late. The story behind why drugs get pulled is more complex than most people realize. It’s not just about bad batches or manufacturing errors. It’s about science, timing, bureaucracy, and the real human cost of delayed action.
How a Drug Gets Approved-And What Happens After
When a new drug hits the market, it’s because the FDA decided its benefits outweigh its risks. That decision is based on clinical trials, often involving thousands of patients. But those trials don’t last forever. They’re limited in scope, duration, and patient diversity. That’s why some problems only show up after thousands-sometimes millions-of people start taking the drug.
That’s where accelerated approval comes in. This pathway lets drugs reach patients faster, especially for serious illnesses like cancer or rare diseases. Instead of waiting for proof that a drug extends life, the FDA may approve it based on a surrogate marker-like tumor shrinkage. It’s a gamble. The company must then prove in follow-up studies that the drug actually helps patients live longer or feel better. If they don’t? The drug gets pulled.
Between 2010 and 2020, about 12.7% of drugs approved through this fast-track route were later withdrawn. In one small cell lung cancer drug, 41% of eligible patients received it-even though it didn’t improve survival. That’s not a rare case. It’s a pattern.
The Long Wait: Why Withdrawals Take Years
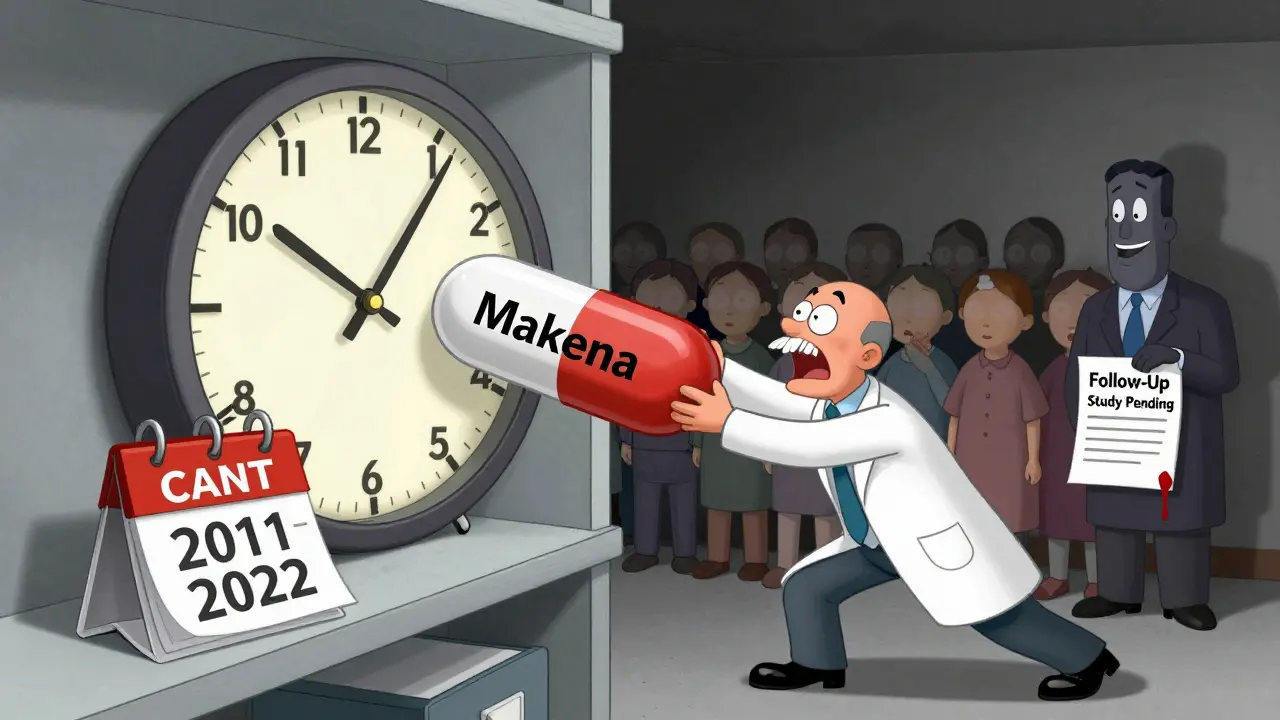
Here’s the shocking part: it used to take the FDA an average of 46 months-almost four years-to pull a drug after evidence showed it didn’t work. Compare that to the approval timeline. The drug Makena, for example, was approved in 2011 based on a single small study. It wasn’t until 2022-11 years later-that the FDA finally withdrew it after a major trial proved it had no benefit for preventing preterm birth. During those 11 years, around 150,000 women received it.
Why the delay? For years, the FDA had no clear legal tool to force a withdrawal quickly. Even when a company failed to complete its required follow-up study, the agency had to go through lengthy hearings, public comment periods, and appeals. Sponsors could drag things out. Patients kept getting the drug. Doctors kept prescribing it.
One oncologist from the Sarah Cannon Research Institute found that 30% of her patients between 2015 and 2020 were on drugs later withdrawn. “We thought we were doing the right thing,” she said. “Turns out, we were giving them hope with no real benefit.”
The 2023 Fix: A New Way to Act Faster
In December 2023, Congress gave the FDA new power. The Consolidated Appropriations Act created a streamlined process to pull drugs that fail their post-approval studies. Now, if a company doesn’t do its required follow-up research, if the study fails to prove benefit, if outside evidence shows harm, or if the company lies in its marketing-the FDA can move fast.
The new process isn’t perfect, but it’s faster. The FDA now has a dedicated team of 12 scientists and doctors just for these cases. Their goal? Cut withdrawal time from 46 months to under 12. The first drug pulled under this new rule was an ALS treatment in August 2023. It took just months-not years.
What changed? The FDA no longer has to wait for a sponsor to voluntarily pull the drug. They can act. They must notify the company, give them a chance to respond, and hold a meeting-but they don’t need to wait for years of legal back-and-forth.
Who Gets Hurt When a Drug Stays Too Long
It’s not just the patients. It’s their families. It’s the doctors who trusted the system. It’s the pharmacists who kept filling prescriptions without knowing the drug had been flagged.
On Reddit’s r/oncology, a thread asking “How many of you have been on drugs later withdrawn?” got over 140 comments. Most were angry. One wrote: “I was on a drug for 18 months. My oncologist said it was standard. Now I’m told it didn’t help. I lost 18 months of my life.”
Patients with metastatic breast cancer, rare cancers, and neurological conditions were especially vulnerable. These are people with few options. When a drug gets approved fast, they’re desperate enough to try it-even if the evidence is shaky. And when it’s pulled years later, they’re left with no backup plan.
Healthcare providers say it takes an average of 72 hours to switch a patient to a new treatment after a drug is withdrawn. That’s not enough time to find alternatives, especially for rare conditions.
Voluntary vs. Mandatory Withdrawals: What’s the Difference?
Not all withdrawals are the same. There are two main types:
- Voluntary withdrawal: The drug company decides to stop selling it. Maybe sales are low. Maybe they found a better drug. Or maybe they’re avoiding a public fight with the FDA. This doesn’t always mean the drug is unsafe.
- Mandatory withdrawal: The FDA orders it. This is the big one. It happens because the drug is unsafe, ineffective, or the company broke the rules. This is what people mean when they say “the drug was pulled.”
The FDA’s guidance says a temporary shortage-like a factory delay-isn’t a withdrawal. Only if the stoppage is because of safety or effectiveness does it count. That distinction matters. A pharmacy might run out of a drug for months and still list it as available. But if the FDA says it’s withdrawn, that’s a red flag.

What You Should Know as a Patient
Here’s the practical side: How do you know if your drug is at risk?
- If you’re on a cancer drug, rare disease treatment, or something approved after 2015, check if it went through accelerated approval. You can ask your doctor or look up the drug on the FDA’s Orange Book-a public list that now includes withdrawal status.
- Don’t assume “FDA-approved” means “forever safe.” Approval is the start, not the end.
- If your doctor prescribes a new drug with limited long-term data, ask: “Has this been through a confirmatory trial? What happens if it fails?”
- Sign up for FDA safety alerts. They send out emails and post updates on their website. You don’t need to be a doctor to understand them.
Pharmacists are also getting better at flagging withdrawn drugs. A 2022 survey found 63% struggled to read the Orange Book listings. Now, with clearer FDA notices and digital alerts, that’s improving. But you shouldn’t rely on them alone.
What’s Next? Real-World Evidence and Faster Decisions
The FDA is now testing a new tool: real-world data. Instead of waiting for a five-year trial, they’re using medical records from hospitals and clinics to track how patients actually do on a drug after it’s approved. A pilot program using data from Flatiron Health is already helping spot drugs that aren’t working.
Experts predict a 25% jump in withdrawals between 2023 and 2027. That doesn’t mean more drugs are dangerous. It means the system is finally catching up. The Makena case exposed a broken process. The 2023 law fixed it.
Some drug companies worry this will scare off innovation. If regulators pull drugs too fast, will they stop approving new cancer treatments? Maybe. But patient advocates say the cost of inaction is worse. “We don’t want drugs pulled because they’re risky,” says the Cancer Research Institute. “We want them pulled because they don’t work.”
Final Thought: Trust, But Verify
Medications save lives. But they can also harm them-especially when we assume approval is a guarantee of safety. The system is improving. It’s faster, clearer, and more transparent than ever before. But you still need to be your own advocate.
Ask questions. Check updates. Don’t assume your doctor knows everything. And if your drug was approved under accelerated approval, stay informed. The next time a drug is pulled, you won’t be caught off guard.







Siobhan K.
So let me get this straight - we let pharmaceutical companies sell drugs based on tumor shrinkage, then wait a decade to find out they don’t actually help people live longer? And we call this progress? I’ve seen this play out with my mother’s breast cancer treatment. She was on a drug that got pulled five years after she stopped taking it. By then, it was too late to try anything else. No one apologized. No one even acknowledged it.
Brian Furnell
It’s critical to distinguish between accelerated approval pathways and the subsequent confirmatory trial mandates - the regulatory architecture here is fundamentally misaligned with clinical reality. The surrogate endpoint paradigm, while expedient, creates a structural incentive for post-marketing non-compliance, particularly when financial stakes are high and enforcement mechanisms are historically under-resourced. The 2023 legislative intervention represents a necessary corrective, but systemic risk remains unless transparency is institutionalized via mandatory real-time adverse event aggregation.
Grace Rehman
Wow so we’re just now fixing this after 10 years of people getting false hope? How many more people have to suffer before we realize that ‘FDA approved’ doesn’t mean ‘good for you’? It’s not rocket science. If it doesn’t work, pull it. Why is this even a debate?
Jackie Be
I had a friend on that ALS drug that got pulled last year - she was so excited because her neurologist said it was ‘the future’ and now she’s in hospice and they’re like oh btw that thing didn’t even work?? I’m so mad I could scream
Ben Warren
It is an incontrovertible fact that the current pharmaceutical regulatory framework exhibits profound structural deficiencies, particularly in the domain of post-marketing surveillance and enforcement efficacy. The protracted latency between the identification of therapeutic futility and the initiation of withdrawal proceedings constitutes a manifest failure of institutional accountability. Furthermore, the historical reliance upon voluntary corporate compliance as a primary mechanism for drug removal is not merely inadequate - it is ethically indefensible. The 2023 legislative amendment, while commendable in intent, remains insufficient without the establishment of binding penalties for non-compliance with confirmatory trial obligations.
Sandy Crux
Let’s be honest - this isn’t about patient safety. It’s about the FDA finally being pressured into doing something because the public finally noticed. The real scandal? The fact that these drugs were ever approved in the first place. Accelerated approval? More like accelerated exploitation. And don’t get me started on how ‘real-world evidence’ is just a fancy way of saying ‘we’re too lazy to run proper trials’.
Hannah Taylor
you know what they dont want you to know right? the FDA is owned by big pharma. they approve the drugs on purpose so they can pull them later and make you pay for new ones. its all a money scheme. i know someone who got cancer from a drug that got pulled. they said it was ‘rare side effect’ but its not rare if they knew and still sold it. they’re killing us slowly
Jay lawch
Western medicine is a scam. In India, we have been using natural remedies for thousands of years. No one dies from ‘side effects’ because we don’t inject chemicals into our bodies. You people are so brainwashed by corporate labs that you think a pill is better than turmeric. This whole system is designed to keep you dependent. The FDA doesn’t care about you - they care about profits. And now they’re pretending to fix something they created? Pathetic.
Michael Ochieng
As someone who’s worked in public health across three continents, I’ve seen how this plays out differently. In the U.S., it’s all about legal liability and corporate lobbying. In places like Ghana or Bangladesh, patients get no access at all - so they take whatever’s available, even if it’s expired or unapproved. The real tragedy isn’t the withdrawal - it’s the fact that most of the world never even gets the chance to be part of this broken system.
Dan Adkins
It is imperative to underscore that the regulatory apparatus governing pharmaceuticals in the United States remains fundamentally compromised by institutional inertia and corporate capture. The withdrawal process, even post-2023, continues to exhibit a marked deficiency in procedural expediency, particularly when compared to the velocity of market entry. Furthermore, the absence of a centralized, real-time pharmacovigilance network - accessible to both clinicians and patients - perpetuates a state of informational asymmetry that is both ethically untenable and clinically hazardous.
Erika Putri Aldana
so like... drugs are just a scam? i mean i get it but like... why do we even have doctors if they just give us stuff that gets pulled later? also why do i have to pay for this? i’m tired
Adrian Thompson
They’re pulling drugs because they’re not working? LOL. What about the ones that are working but they’re pulled because they’re too cheap? Like, you think the FDA gives a damn about patients? They care about patent cliffs and making sure the next $200k-a-year drug gets approved. This whole thing is rigged. And don’t even get me started on how they’re using ‘real-world data’ to justify more surveillance.
Orlando Marquez Jr
The consolidation of regulatory authority under the FDA, while ostensibly enhancing oversight, necessitates a concomitant expansion of technical and analytical capacity. The establishment of a dedicated withdrawal review team represents a positive institutional adaptation. However, the efficacy of this initiative will be contingent upon sustained funding, interagency data integration, and the formal incorporation of patient-reported outcomes into the evidentiary standard for withdrawal decisions. Without these components, the reform remains procedural rather than substantive.