For years, fish oil supplements have been touted as a simple way to protect your heart. Walk into any pharmacy, and you’ll see shelves packed with bottles promising lower cholesterol, reduced inflammation, and fewer heart attacks. But here’s the truth: the science is messy. Some studies say fish oil saves lives. Others say it does almost nothing. So what’s actually going on?
What Exactly Are Omega-3s?
Omega-3 fatty acids are essential fats your body can’t make on its own. The two most important types for heart health are EPA (eicosapentaenoic acid) and DHA (docosahexaenoic acid). These are found mostly in fatty fish like salmon, mackerel, sardines, and anchovies. There’s also ALA, a plant-based version in flaxseeds and walnuts, but your body converts very little of it into EPA or DHA-so it doesn’t count as a reliable source for heart protection.
Most fish oil supplements contain both EPA and DHA, usually around 300-500 mg per capsule. But here’s the catch: the doses used in major heart studies were much higher. The REDUCE-IT trial, which showed strong benefits, used 4 grams of pure EPA daily. That’s eight to ten standard fish oil pills. Most people never take that much.
The Big Studies: Contradictory Results
In 2018, the REDUCE-IT trial shook the medical world. It followed nearly 8,200 people with high triglycerides and existing heart disease or diabetes. All were already on statins. Half took 4 grams of pure EPA (Vascepa) daily. The other half took a placebo made of mineral oil. After five years, the EPA group had 25% fewer heart attacks, strokes, and heart-related deaths. This wasn’t a small effect-it was dramatic.
Then came STRENGTH in 2020. This trial used the same high dose-4 grams daily-but with a mix of EPA and DHA. The results? Nothing. No benefit. The trial was stopped early because it was clear the supplement wasn’t working. Why the difference? Researchers think DHA might cancel out some of EPA’s benefits. Or maybe the mineral oil placebo in REDUCE-IT actually worsened outcomes, making EPA look better than it was.
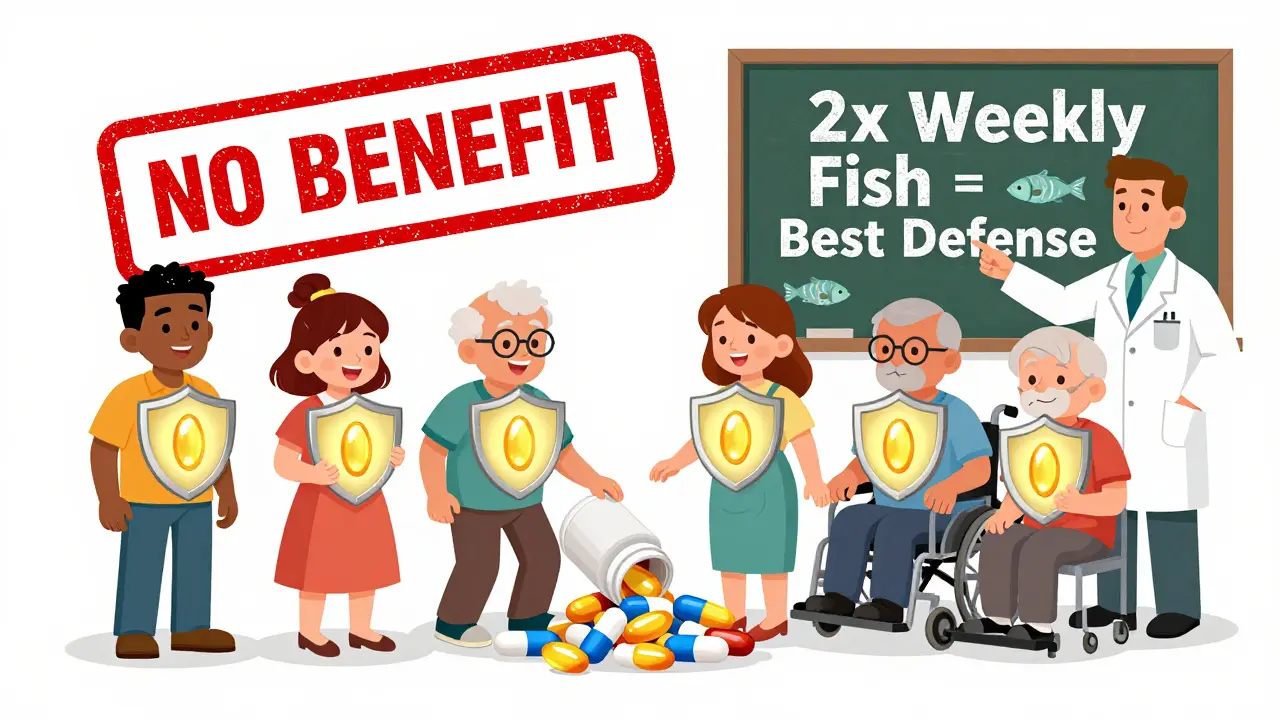
In 2023, the Cochrane Collaboration reviewed 79 trials with over 112,000 people. Their conclusion: long-chain omega-3s (EPA and DHA) have little to no effect on heart disease risk for the average person. That’s the largest, most rigorous analysis ever done. And it found no meaningful benefit from supplements.
Who Might Still Benefit?
Not everyone. The data isn’t useless-it’s just selective.
People with very high triglycerides (above 500 mg/dL) still get real benefit from prescription omega-3s like Vascepa or Lovaza. These are FDA-approved for that specific use. For them, lowering triglycerides by 25-30% matters. High triglycerides are a known risk factor for pancreatitis and heart disease.
The VITAL trial found something surprising: in African Americans, taking 1 gram of omega-3s daily cut heart attacks by 77%. That’s a massive difference. Researchers think it may be linked to genetic differences in how the body processes omega-3s. This isn’t just a fluke-it’s a pattern seen in multiple studies.
People with heart failure also seem to benefit slightly. The American Heart Association says omega-3 supplements may reduce death from heart failure by about 10%. That’s not a cure, but it’s something.
Prescription vs. Over-the-Counter: Big Differences
Not all fish oil is created equal. There’s a huge gap between what you buy at the grocery store and what doctors prescribe.
- Over-the-counter fish oil: Usually 300-500 mg EPA+DHA per capsule. You’d need 8-10 capsules daily to match the REDUCE-IT dose. Quality varies. Some brands have oxidized oil (rancid), which can be harmful. Consumer Reports found 12 out of 35 popular brands failed oxidation tests.
- Prescription Vascepa: Pure EPA, 1 gram per capsule. Taken twice daily. FDA-approved for high-risk patients with high triglycerides. Costs around $300/month with insurance.
- Prescription Lovaza: Mix of EPA and DHA. Only approved for triglycerides above 500 mg/dL. Not for preventing heart attacks.
Most people taking fish oil supplements are using the over-the-counter kind. That’s not the same as what worked in REDUCE-IT. It’s like comparing a bicycle to a race car and wondering why the bike didn’t win the Tour de France.
What About Eating Fish Instead?
The best way to get omega-3s isn’t from a pill-it’s from food. The American Heart Association recommends two 3.5-ounce servings of fatty fish per week. That gives you about 500 mg of EPA+DHA daily-the amount linked to lower heart disease risk in population studies.
Salmon, sardines, herring, trout, and mackerel are top choices. Canned tuna has some, but less than wild-caught salmon. Farmed salmon has more fat but also more contaminants like PCBs, so variety matters.
And here’s the kicker: people who eat fish regularly have lower rates of heart disease-even if they don’t take supplements. That suggests fish oil isn’t the magic ingredient. It’s the whole food: omega-3s, protein, vitamin D, selenium, and the fact that people who eat fish often eat less processed meat and junk food.
The Downsides: Side Effects and Risks
Fish oil isn’t harmless. At high doses, it can cause:
- Fishy burps or aftertaste (reported by 32% of users)
- Stomach upset, diarrhea, nausea (27% of users)
- Increased risk of atrial fibrillation (a type of irregular heartbeat). A 2022 meta-analysis found a 0.4% absolute increase in risk at doses over 4 grams daily.
- Potential bleeding risk, especially if you’re on blood thinners like warfarin. The risk is small at normal doses, but it’s real.
Some supplements are contaminated with mercury or PCBs, but reputable brands test for this. Look for third-party certifications like USP, NSF, or ConsumerLab.
What Do Doctors Actually Recommend Now?
Cardiologists’ opinions have shifted sharply since 2018. A 2024 survey on Medscape found that 68% of cardiologists no longer recommend fish oil supplements for primary prevention (meaning people without heart disease).
But they still prescribe Vascepa to high-risk patients: those with diabetes and high triglycerides, or those who’ve already had a heart attack and still have high triglycerides despite statins. For them, the benefit is clear.
For the rest of us? The American Heart Association’s current stance is simple: don’t rely on supplements. Get your omega-3s from food. If you have high triglycerides, talk to your doctor about prescription options. If you’re healthy and eating fish twice a week, you’re probably fine.
The Bottom Line
Fish oil supplements aren’t a magic bullet. For most people, they don’t prevent heart attacks or strokes. But for a specific group-those with high triglycerides, heart failure, or certain genetic backgrounds-they can make a real difference.
Don’t waste money on cheap fish oil pills hoping for protection. If you don’t eat fatty fish regularly, start there. Try salmon on the grill once a week. Add sardines to your salad. That’s cheaper, safer, and more effective than any supplement.
If you have heart disease or high triglycerides, talk to your doctor. You might need Vascepa-not a bottle from the pharmacy. And if you’re taking high doses, get your liver and heart rhythm checked. Omega-3s aren’t risk-free.
The science isn’t settled, but the direction is clear: context matters. Who you are. What your numbers are. What you eat. That’s what determines whether fish oil helps-or just fills your medicine cabinet.







Tru Vista
fish oil? lol. just eat salmon. done. also, your supplements are probably rancid anyway. 🤡
erica yabut
Oh sweet mercy, another person who thinks popping pills is a substitute for actual dietary wisdom. You know what’s cheaper than $300/month Vascepa? A fork. And a grill. And the courage to eat food that doesn’t come in a plastic bottle labeled ‘heart-healthy’ like it’s a TikTok trend. Your body isn’t a vending machine. Stop treating omega-3s like a magic bullet and start treating them like the nuanced biochemicals they are. Also, your fishy burps? That’s your body screaming, ‘I didn’t sign up for this.’
Vincent Sunio
It is, however, a matter of considerable scientific interest that the REDUCE-IT trial utilized purified EPA, whereas STRENGTH employed a combination of EPA and DHA - a critical distinction often obfuscated by popular media. The placebo arm in REDUCE-IT, composed of mineral oil, may have induced pro-inflammatory effects, thereby artificially inflating the relative efficacy of EPA. This confounder, while acknowledged in peer-reviewed commentary, remains under-discussed in lay discourse. The Cochrane meta-analysis, by contrast, employed rigorous heterogeneity controls and remains the most statistically robust evidence to date.
Palesa Makuru
Okay but like… why are we still talking about fish oil like it’s a lifestyle choice? I’m from South Africa, we don’t have salmon in the freezer aisle like you guys. We eat sardines straight from the tin with chili and onions - cheap, local, delicious. And guess what? Our heart disease rates are lower than yours. Maybe it’s not the omega-3s. Maybe it’s not taking your food and turning it into a supplement you can swallow while scrolling Instagram. Just eat real food. Stop overthinking it. 🌍
Ian Ring
I’ve been taking fish oil for 7 years… and honestly? I feel fine. Not ‘miracle energy’ fine, just… not worse. I think the problem isn’t the supplement - it’s the expectation. We want magic. But biology doesn’t work like that. Also, I use Nordic Naturals. No fish burps. Ever. 🙌
Shanahan Crowell
Let’s all just chill for a sec. The science is messy? Yeah. But that’s science. It’s not a TikTok trend. It’s not a cult. It’s data. And data says: if you’re healthy, eat fish. If you’re high-risk, talk to your doc. If you’re just buying pills because your cousin said it ‘cleansed her arteries’ - maybe pause. This isn’t about being right. It’s about being smart. And being kind to your body. 💚
Tiffany Channell
Let’s not forget the elephant in the room: Big Pharma funded REDUCE-IT. Vascepa is a billion-dollar drug. STRENGTH? Funded by a different pharma. Coincidence? Or is this just another case of industry shaping evidence to fit a profit model? The Cochrane review? Independent. No conflict. And it says: nothing. Not even a whisper. Wake up.
Hank Pannell
What’s fascinating here isn’t whether omega-3s work - it’s how we’ve turned a biological nutrient into a moral binary. If you take supplements, you’re naive. If you don’t, you’re reckless. If you eat fish, you’re virtuous. If you don’t, you’re lazy. But health isn’t a virtue signaling contest. It’s a complex interplay of genetics, environment, access, culture, and luck. The fact that African Americans saw a 77% drop in heart attacks? That’s not noise - that’s a signal we’re ignoring because it doesn’t fit the tidy narrative. Maybe the answer isn’t ‘more pills’ or ‘less pills’ - but ‘more research on who benefits, and why.’
Lori Jackson
Ugh. I knew it. Another ‘eat fish’ post. Like, wow, revolutionary. Meanwhile, my mom’s triglycerides are 800, she’s on statins, and her doctor prescribed Vascepa - and it dropped them to 300. So yes, for some people, it’s life-changing. But you? You’re just here to feel superior because you bought wild-caught salmon once. Grow up. Not everyone has the time, money, or access to be a ‘foodie’ wellness influencer. Some of us need science-backed medicine. Not a Pinterest board.
Sarah Little
Just a note: the oxidized oil issue is real. I bought a popular brand last year and my fridge smelled like a seafood market in July. I threw it out. No one talks about this. Also, did you know some brands use fish from overfished waters? You’re not saving your heart - you’re destroying oceans. So… maybe just eat tofu?
innocent massawe
Back home in Nigeria, we fry small fish with peppers and eat them whole - bones and all. No pills. No fancy labels. Just food. My uncle, 78, still carries firewood. No heart issues. Maybe the answer isn’t in capsules. Maybe it’s in rhythm. In community. In eating what’s around you, not what’s marketed to you.
JUNE OHM
THIS IS A BILLION-DOLLAR SCAM. 🤫 Fish oil? HA. The FDA knows. The WHO knows. But they’re too scared to say it. Why? Because if people stop buying pills, the whole ‘supplement industry’ collapses. And who profits? The meat industry. The processed food giants. They want you weak. They want you dependent. Eat real food? Nah. That’s too hard. So they sell you bottles of ‘heart magic’ made from fish that’s been sitting in a warehouse for 18 months. 💀
Philip Leth
My abuela in Mexico used to make this soup with dried shrimp and hominy. Said it ‘cleansed the blood.’ Didn’t know about EPA. Didn’t need to. She just knew what worked. Food isn’t a supplement. It’s memory. It’s culture. It’s love. You can’t bottle that. And you shouldn’t try.
Kerry Howarth
Don’t overcomplicate it. If you eat fish twice a week, you’re golden. If you don’t, get a prescription if you’re high-risk. Otherwise, save your money. And your liver. Simple. Clear. Done.
Brittany Wallace
It’s funny how we turn everything into a debate. The truth? We’re all just trying to survive. Some of us have the luxury to grill salmon. Others are choosing between rent and fish oil. The real question isn’t ‘does it work?’ - it’s ‘how do we make real health accessible?’ Maybe that’s the real omega-3 we’re missing.