What You’re Really Seeing When You Look at a Rash
Two people walk into a clinic with red, itchy patches on their skin. One has eczema. The other has psoriasis. They look similar at first glance-red, flaky, annoying. But if you know what to look for, the differences jump out. And getting it wrong? That means using the wrong treatment, wasting months, and making the condition worse.
According to a 2022 study in the Journal of the American Academy of Dermatology, about 1 in 5 cases of eczema and psoriasis are misdiagnosed. That’s not because doctors are careless. It’s because the visual clues are subtle, especially on darker skin tones. And most of us-patients included-have only seen textbook images of red, scaly patches on pale skin. Real life doesn’t look like that.
Location: Where the Rash Lives Tells You Everything
The first thing to check? Where the rash is sitting on the body.
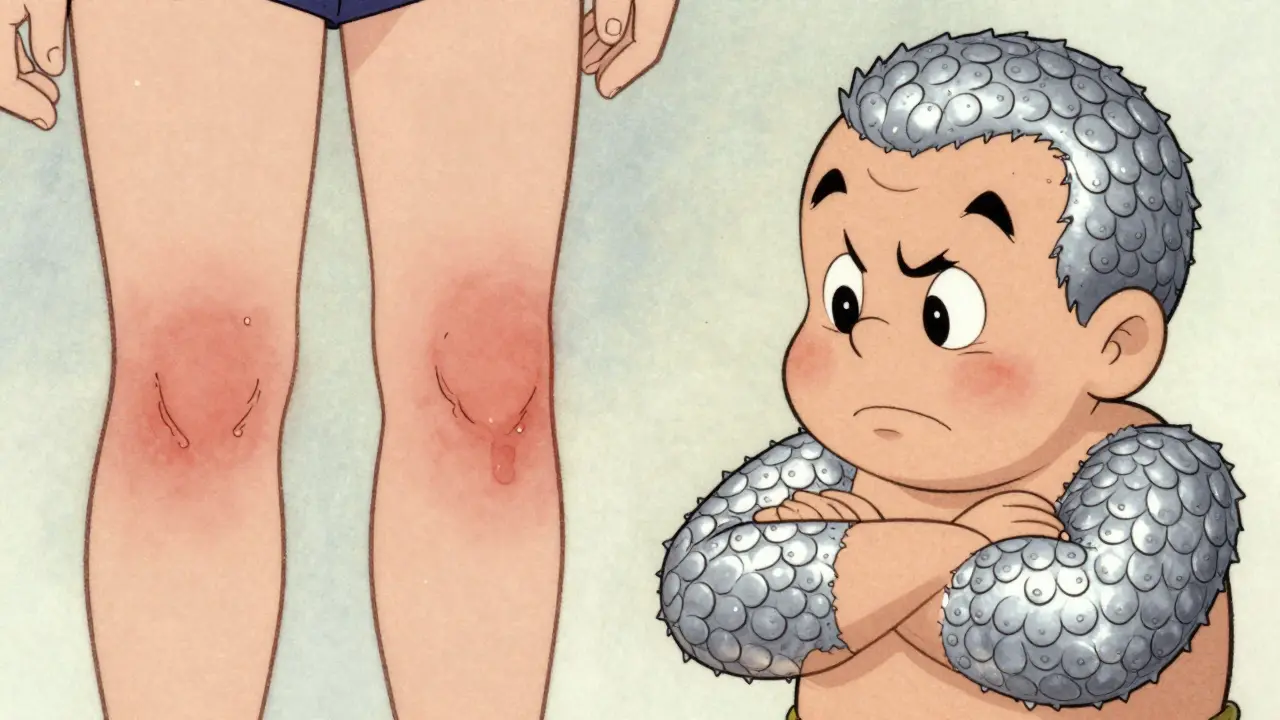
Eczema loves the bends. The inside of your elbows? That’s ground zero. Behind the knees? Almost as common. You’ll often see it on the wrists, ankles, neck, and in babies, the cheeks and forehead. It’s the skin that folds, creases, or rubs against clothes. It’s not random-it’s the body’s reaction to irritation, dryness, and allergens.
Psoriasis? It’s the opposite. It shows up on the outsides. The outer elbows, the front of the knees, the scalp, the lower back. These are the bony, exposed areas. If you have thick patches on your scalp that look like dandruff but won’t brush off, or a patch on your lower back that won’t fade even after moisturizing, it’s more likely psoriasis.
A 2020 study of over 1,200 patients found that 95% of eczema cases involved skin folds. Only 12% of psoriasis cases did. And 89% of psoriasis cases were on the outer joints-where eczema rarely shows up. That’s not a coincidence. It’s a pattern.
Texture: Flaky vs. Oozing vs. Armor-Like
Now look closer at the surface.
Eczema often looks raw. In its acute phase, the skin may weep, crust, or even bleed from scratching. It’s not dry-it’s broken. The edges are blurry, like a watercolor painting that’s run. The scales, if there are any, are fine and powdery. In chronic cases, the skin gets thick and leathery from constant rubbing-that’s called lichenification. But it’s still soft to the touch.
Psoriasis is different. It’s like armor. The patches are raised, well-defined, and covered in thick, silvery-white scales. These aren’t loose flakes. They’re stuck on tight. If you gently scrape one with a glass slide, you might see pinpoint bleeding underneath-that’s the Auspitz sign, a hallmark of psoriasis. You won’t see that with eczema.
And here’s something most people miss: psoriasis scales are about five times thicker than eczema scales. One study measured them at 0.5mm versus 0.1mm. That’s not just a difference in appearance-it’s a difference in biology. Psoriasis is a speed-up of skin cell production. Eczema is a breakdown of the skin barrier.
Color: It’s Not Just About Red
Most pictures of eczema and psoriasis show bright red patches on white skin. But that’s not what it looks like on darker skin tones.
On skin of color, eczema doesn’t always look red. It can appear as ashen, purple, or gray patches. The redness is masked by melanin. The skin may look darker or lighter than the surrounding area, with subtle scaling that’s easy to miss. Many patients with darker skin are told they just have dry skin-for years.
Psoriasis on darker skin isn’t silvery-white either. It’s more likely to be violet, deep brown, or gray. But the scales? Still there. Still thick. Still stuck. And the borders? Still sharp. That’s the key. Even when the color changes, the shape stays clear.
A 2021 study in JAMA Dermatology found that dermatologists misdiagnose eczema and psoriasis in patients with Fitzpatrick skin types IV-VI up to 35% more often than in lighter skin. Why? Because medical training still relies on images of pale skin. That’s changing-slowly-but if you’re a patient with darker skin, you need to know what to look for.

Nails and Trauma: The Hidden Clues
Look at your nails. Really look.
Psoriasis loves the nails. Half of people with psoriasis develop tiny pits-like pinpricks-in the nail plate. The nail might lift away from the bed. It might crumble or change color. Eczema? Rarely affects nails. If it does, you might see ridges or discoloration, but never true pitting.
Another clue? Trauma. If you scratch your skin, get a cut, or even wear tight jewelry, and new patches show up right where the injury happened? That’s the Koebner phenomenon. It happens in 25-30% of psoriasis patients. It’s rare in eczema.
And don’t ignore the scalp. Psoriasis on the scalp looks like thick, scaly plaques that extend beyond the hairline. Eczema on the scalp is usually flaky and oily, more like seborrheic dermatitis. It doesn’t form thick, raised plaques.
What Patients Say: The Real-Life Visual Experience
Patients don’t describe these conditions with medical terms. They use their own words.
On eczema forums, people say: “It looks like my skin is raw,” “It bleeds when I rub it,” “It oozes at night.” One person wrote, “It’s like my skin forgot how to be skin.”
On psoriasis forums? “It looks like armor,” “Like someone glued silver paper to my skin,” “I can see the scales from across the room.” Another said, “I don’t care if it’s itchy-I care that people stare.”
A 2022 study found that psoriasis patients were over three times more likely to say their rash looked “visibly different” from normal skin. Eczema patients? They said their rash blended in-until it cracked open.
How to Tell at Home (Without a Doctor)
You don’t need a microscope to spot the difference. Here’s what you can do:
- Check the location. Is it in the bends? Eczema. On the outsides? Psoriasis.
- Look at the scales. Fine and powdery? Eczema. Thick, silvery, stuck on? Psoriasis.
- Try the scale test. Gently scrape with a glass slide or fingernail. If you see tiny red dots underneath? That’s psoriasis.
- Check your nails. Pitting? Psoriasis. Ridges? Maybe eczema, but unlikely.
- Watch the color. On darker skin, don’t wait for red. Look for sharp borders and thick scale.
And take photos. Same light, same angle, same time of day. Psoriasis stays stubbornly the same. Eczema changes with weather, stress, soap, laundry detergent. Tracking that helps.

The New Tech-And Why It’s Not a Replacement
In January 2024, the FDA approved the first AI tool that can analyze smartphone photos to guess whether it’s eczema or psoriasis. It’s 85% accurate.
But here’s the catch: it’s only 63% accurate on darker skin tones. Why? Because the AI was trained mostly on images of light skin. That’s not a glitch-it’s a systemic flaw.
Some clinics now use multispectral imaging, which reads how skin reflects different wavelengths of light. Psoriasis and eczema have different patterns. This tech is 93% accurate in research settings.
But no app, no algorithm, no camera replaces a trained eye. Especially when you’re dealing with skin of color. That’s why dermatology residencies now require 40 hours of skin of color training-up from just 8 in 2019. The field is catching up.
When to See a Dermatologist
If your rash lasts more than two weeks, gets worse with moisturizers, or spreads despite avoiding known triggers, see a dermatologist. Don’t wait. Misdiagnosis leads to delayed treatment, unnecessary stress, and sometimes permanent skin changes.
Bring your photos. Note when it flares. Mention if you have joint pain (psoriasis can link to arthritis). Tell them if you’ve been told it’s “just dry skin” before. And if you have darker skin, ask: “Have you seen this condition on skin like mine?”
There’s no shame in asking. The right diagnosis isn’t just about treatment-it’s about dignity. Your skin matters. Your experience matters. And you deserve to be seen correctly.
Final Thought: It’s Not About Labels. It’s About Relief.
Whether it’s eczema or psoriasis, both are chronic. Both can be managed. Both can flare. Both can feel isolating.
But knowing which one you have? That’s the first step to real control. Not guesswork. Not trial and error. Not waiting months for someone to notice the difference.
The visual clues are there. You just need to know where to look-and who to trust.






Kacey Yates
Eczema is raw psoriasis is armor period. Stop moisturizing psoriasis like its dry skin its literally growing too fast. I got misdiagnosed for 3 years and now my skin looks like reptile scales. No joke.
Laura Arnal
This is so helpful 😊 I finally understand why my rash never improved with lotion! I thought I was just bad at skincare. Time to see a derm who actually knows skin of color!
Megan Brooks
The distinction between barrier dysfunction and hyperproliferation is clinically profound. While layperson observation is valuable, it must be contextualized within the broader biopsychosocial model of dermatologic care. Misdiagnosis disproportionately impacts marginalized populations due to systemic educational gaps.
Ryan Pagan
Psoriasis doesn't just sit there like some stubborn tattoo-it *demands* attention. I've had scales so thick I could hear them crack when I moved. And yeah, the nail pitting? That's the silent scream you can't ignore. Eczema whispers. Psoriasis roars.
Paul Adler
I appreciate the emphasis on visual differences and the caution against over-relying on AI. Skin diversity isn't a footnote-it's the whole textbook. I've seen too many patients dismissed as 'just dry' when it was clearly psoriasis. The Koebner phenomenon alone should be taught in high school bio.
rajaneesh s rajan
So you're telling me my 'dandruff' on scalp is actually armor? And my doctor called it 'seasonal flaking'? Bro. I paid 200 bucks for a dermatologist who Google-searched my symptoms. India has zero dermatologists who've seen psoriasis on brown skin. We're all just guessing.
ryan Sifontes
AI got 85% accuracy? Lmao. They trained it on 10k pics of white people and now they want us to trust it? Next they'll say the sun doesn't cause cancer because the model says so. This is just Big Pharma letting algorithms do the dirty work.
Jasneet Minhas
I used to think my skin was just 'dark and dry' until I saw a pic of my own rash side by side with a psoriasis textbook image. Same pattern. Same borders. Different color. 🤦♂️ Now I send every derm this article. They either nod or say 'I'll look into it.'
Eli In
I'm from Nigeria and we have zero resources for this. My cousin was told she had 'allergic reaction' for 5 years. When she finally got diagnosed with psoriasis, she cried because she thought she was contagious. This post should be translated into 10 languages.
Kristie Horst
It is, indeed, a matter of dignity. The systemic neglect of pigmented skin in dermatological education is not merely an oversight-it is a form of epistemic violence. One cannot diagnose what one has never been taught to see.
LOUIS YOUANES
I don't need a 40-hour course. I just need someone who didn't graduate from a university that still uses 1998 textbooks. If you're still teaching 'red patches' as the gold standard, you're not a doctor-you're a relic.
Keith Oliver
You think this is bad? Wait till you see the AI that diagnoses depression from selfies. At least this one's 85% accurate. The rest of medicine? 30% if you're lucky. I'd rather have a 12-year-old with a phone than a dermatologist who thinks melanin is just a filter.