Dulcolax vs Alternatives Comparison Tool
Side-by-Side Comparison Table
| Product | Onset (hours) | Mechanism | Typical Oral Dose | Common Side-Effects | Cost (AU$ per pack) | OTC Availability |
|---|---|---|---|---|---|---|
| Dulcolax (bisacodyl) | 6-12 | Stimulant - irritates colon wall | 5 mg tablet once daily (max 10 mg) | Abdominal cramp, urgency | ~$8-$12 | Yes |
| Senna | 6-12 | Stimulant - bacterial conversion of sennosides | 17.2 mg tablet (2-3 mg sennosides) once daily | Cramping, possible discoloration of stool | ~$6-$10 | Yes |
| Milk of Magnesia | 12-24 | Osmotic - draws water into colon | 30 mL liquid, 2-4 times daily | Flatulence, mild electrolyte shift | ~$5-$9 | Yes |
| Polyethylene Glycol 3350 | 24-48 | Osmotic - retains water in stool | 17 g powder dissolved in 250 mL water daily | Bloating, rare allergic rash | ~$12-$18 | Yes |
| Psyllium Husk | 24-72 | Bulk-forming - absorbs water, adds fibre | 5-10 g (1-2 tbsp) mixed with liquid, 1-2×/day | Gas, rare obstruction if not hydrated | ~$7-$11 | Yes |
| Lubiprostone | 24-48 | Chloride channel activator - increases intestinal fluid | 24 µg capsule twice daily | Nausea, headache, abdominal pain | Prescription; ~ $150-$200 per month | No (prescription only) |
Quick Summary
- Dulcolax (bisacodyl) works fast, usually 6‑12hours, but can cause cramps.
- Senna is a plant‑based stimulant with a similar onset, often cheaper.
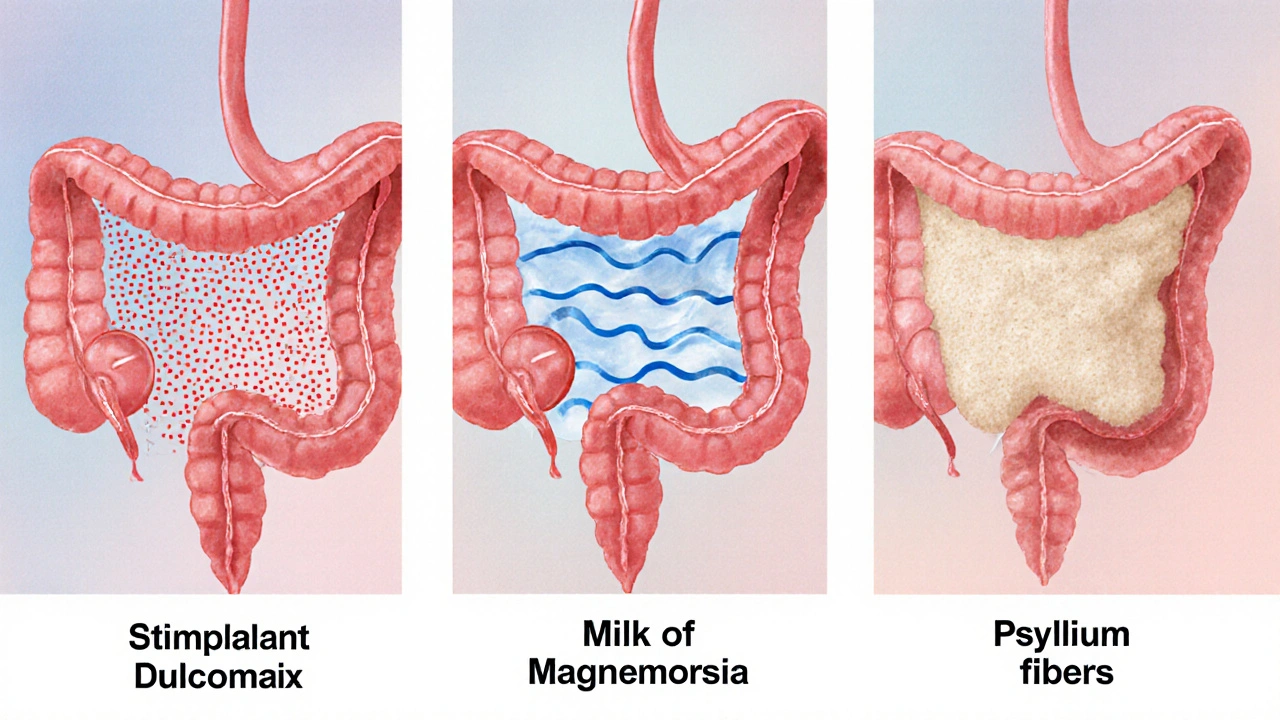
- Milk of Magnesia (magnesium hydroxide) draws water into the colon, acting slower (12‑24hours) and is gentler on the gut.
- Polyethylene glycol (PEG3350) is an osmotic laxative that hydrates stool without cramping, but needs a few days for full effect.
- Fiber supplements like psyllium husk work progressively and are best for long‑term bowel health.
When constipation strikes, the market is packed with options. This guide lines up Dulcolax alternatives side by side so you can pick the right one for your body, budget, and schedule.
Dulcolax is a brand name for bisacodyl, a synthetic stimulant laxative that irritates the lining of the colon to trigger a bowel movement. It’s been on pharmacy shelves since the 1950s and is available as tablets, suppositories, and liquid syrup. The drug works by increasing intestinal peristalsis and fluid secretion, usually delivering relief within 6‑12hours when taken orally.
Why a Comparison Matters
Constipation isn’t one‑size‑fits‑all. Some people need a quick fix, others a gentle, daily routine. Choosing the wrong laxative can mean lingering cramps, dehydration, or even dependence. By comparing key attributes-onset speed, mechanism, typical dose, side‑effects, cost, and OTC status-you’ll see which product fits your lifestyle.
Major Alternatives to Dulcolax
Below are the most widely used over‑the‑counter options you’ll find in Australian pharmacies and supermarkets.
Senna (often sold under brands like Ex-Lax) is a plant‑derived stimulant laxative. Its active compounds, sennosides, are converted by gut bacteria into agents that stimulate colonic muscles.
Milk of Magnesia (magnesium hydroxide) is an inorganic salt that works osmotically, pulling water into the intestinal lumen to soften stool.
Polyethylene Glycol 3350 (commonly known as MiraLAX) is a large‑molecule osmotic agent that retains water in the stool without stimulating the bowel wall.
Psyllium Husk (sold as Metamucil, Metamucil Clear & Fit) is a soluble fiber that expands when mixed with liquid, adding bulk and moisture to stool.
Lubiprostone (brand name Amitiza) is a prescription chloride channel activator that increases intestinal fluid secretion, easing passage of stool.
Sodium Picosulfate (found in Picolax and some bowel‑prep kits) is a pro‑drug stimulant that activates colonic nerves after bacterial conversion.
Side‑by‑Side Comparison Table
| Product | Onset (hours) | Mechanism | Typical Oral Dose | Common Side‑Effects | Cost (AU$ per pack) | OTC Availability |
|---|---|---|---|---|---|---|
| Dulcolax (bisacodyl) | 6‑12 | Stimulant - irritates colon wall | 5mg tablet once daily (max 10mg) | Abdominal cramp, urgency | ~$8‑$12 (10‑tablet pack) | Yes |
| Senna | 6‑12 | Stimulant - bacterial conversion of sennosides | 17.2mg tablet (2‑3mg sennosides) once daily | Cramping, possible discoloration of stool | ~$6‑$10 (10‑tablet pack) | Yes |
| Milk of Magnesia | 12‑24 | Osmotic - draws water into colon | 30mL (≈1tsp) liquid, 2-4times daily | Flatulence, mild electrolyte shift | ~$5‑$9 (200mL bottle) | Yes |
| Polyethylene Glycol 3350 | 24‑48 | Osmotic - retains water in stool | 17g powder dissolved in 250mL water daily | Bloating, rare allergic rash | ~$12‑$18 (210g box) | Yes |
| Psyllium Husk | 24‑72 | Bulk‑forming - absorbs water, adds fibre | 5‑10g (1‑2 tbsp) mixed with liquid, 1‑2×/day | Gas, rare obstruction if not hydrated | ~$7‑$11 (200g pack) | Yes |
| Lubiprostone | 24‑48 | Chloride channel activator - increases intestinal fluid | 24µg capsule twice daily | Nausea, headache, abdominal pain | Prescription; ~ $150‑$200 per month | No (prescription only) |
| Sodium Picosulfate | 6‑12 | Stimulant - pro‑drug activated by gut bacteria | 5mg tablet once daily (max 10mg) | Cramping, urgency | ~$9‑$14 (10‑tablet pack) | Yes (often in bowel‑prep kits) |
How to Choose the Right Option for You
Pick a laxative based on three practical factors:
- Urgency: Need relief tonight? Stimulants like Dulcolax, Senna, or Sodium Picosulfate act within half a day.
- Comfort level: If cramps are a deal‑breaker, go osmotic (Milk of Magnesia, PEG 3350) or fibre (Psyllium) which are gentler.
- Long‑term goals: For chronic constipation, fibre and osmotic agents are safer for daily use; reserve stimulants for occasional rescue.
Also consider medical conditions. Kidney disease can make magnesium‑based products risky, while inflammatory bowel disease patients should avoid harsh stimulants without doctor advice.
Safety Tips and Common Pitfalls
Even over‑the‑counter meds can backfire if misused.
- Don’t exceed the recommended dose. More isn’t faster; it just raises the chance of severe cramping or electrolyte imbalance.
- Stay hydrated. Osmotic laxatives pull water into the gut; without enough fluid you could worsen constipation.
- Avoid daily stimulant use. Habitual use can lead to colon muscle dependence, making the gut lazy.
- Check interactions. Bisacodyl can increase absorption of certain antibiotics; magnesium can interfere with some heart meds.
Cost‑Effectiveness Snapshot
For most Australians, price matters. A quick look:
- Dulcolax and Senna sit at the low‑end (~$8‑$10) and are easy to find at supermarkets.
- Milk of Magnesia is similarly cheap and doubles as an antacid, but you need larger volumes.
- PEG 3350 costs more per dose but provides steady, gentle relief for chronic cases, potentially saving doctor visits.
- Lubiprostone is the pricey prescription‑only option, typically reserved for severe, refractory constipation.
When to See a Doctor
If you notice any of these red flags, stop self‑medicating and consult a GP:
- Bloody or black stools (possible GI bleeding).
- Severe abdominal pain unrelieved by laxatives.
- Constipation lasting more than 2weeks despite treatment.
- Unexplained weight loss, fever, or vomiting.
These symptoms could signal underlying conditions like obstructive lesions, inflammatory bowel disease, or medication side‑effects that need professional care.
Frequently Asked Questions
How fast does Dulcolax work compared to Senna?
Both Dulcolax and Senna are stimulant laxatives, so they usually start working within 6‑12hours after an oral dose. The exact timing can vary with age, diet, and gut flora, but most users notice a bowel movement by the next morning.
Can I take Dulcolax every day?
Doctors generally advise against daily stimulant use because the colon can become dependent on the drug. For chronic constipation, switch to a fibre supplement or an osmotic laxative and reserve Dulcolax for occasional rescue.
Is Milk of Magnesia safe for people with kidney problems?
Magnesium can accumulate in patients with impaired renal function, leading to high serum magnesium levels. Those with kidney disease should choose a non‑magnesium option like PEG 3350 or consult their doctor before using Milk of Magnesia.
What’s the difference between PEG 3350 and Dulcolax?
PEG 3350 is an osmotic laxative that gently retains water in the stool, causing minimal cramping. Dulcolax is a stimulant that irritates the colon wall, leading to quicker results but more abdominal discomfort.
Can I combine a stimulant laxative with a fibre supplement?
Yes, many clinicians advise using a stimulant like Dulcolax for short‑term relief while taking daily fibre (e.g., Psyllium) to maintain regularity. Just be sure to stay well‑hydrated to avoid blockage.






liza kemala dewi
When contemplating the comparative efficacy of bisacodyl relative to its over‑the‑counter counterparts, one must first acknowledge the multifaceted nature of constipation as a physiological condition.
The stimulant action of Dulcolax, mediated through direct irritation of the colonic mucosa, yields a rapid onset that is frequently prized by patients seeking prompt relief.
Conversely, agents such as senna, while sharing a similar temporal profile, derive their activity from bacterial conversion of sennosides, a process that introduces variability contingent upon individual microbiota.
Osmotic laxatives, exemplified by magnesium hydroxide and polyethylene glycol, eschew mucosal irritation in favor of hydro‑electrolytic gradients that draw water into the intestinal lumen.
Such mechanisms, albeit slower in onset, are often lauded for their gentler side‑effect profile, particularly the reduced incidence of crampy abdominal pain.
Nonetheless, the selection of an appropriate agent cannot be reduced to a mere comparison of onset times; considerations of patient comorbidities, such as renal insufficiency, exert profound influence on therapeutic suitability.
For instance, in individuals with compromised renal function, magnesium‑based formulations may precipitate hypermagnesemia, thereby contraindicating their use.
Similarly, chronic reliance on stimulant laxatives raises concerns regarding colonic tachyphylaxis and potential dependence.
From an economic perspective, the price disparity between generic bisacodyl and prescription‑only agents such as lubiprostone is nontrivial, often dictating patient adherence.
Insurance coverage, regional pricing, and pharmacy markup further compound the financial calculus that patients must navigate.
The clinician’s role, therefore, extends beyond pharmacologic recommendation to encompass education on proper dosing, hydration, and the importance of periodic drug holidays.
Moreover, integrating dietary fiber, as represented by psyllium husk, can synergistically augment stool bulk while mitigating reliance on pharmacotherapy.
Evidence suggests that a combined regimen of occasional stimulant use with daily fiber intake may achieve optimal bowel regularity with minimal adverse events.
In summary, Dulcolax offers a rapid, cost‑effective solution for acute constipation, yet its selection should be individualized based on clinical context.
A nuanced, patient‑centered approach remains the cornerstone of effective constipation management.
Jay Jonas
Man, I was like totally shocked when I tried Dulcolax for the first time – the rush came on faster than my morning coffee, no joke!
But then Senna danced in with the same speed, and I swear my gut was having a tiny rave.
The cheap Milk of Magnesia felt like a slow‑mo movie, but it kept things chill, you know?
PEG 3350 was the marathon runner, taking its sweet time but never gave up on the finish line.
Psyllium was the steady friend, building up gradually for that long‑term vibe.
And that pricey Lubiprostone? Yeah, it’s like the VIP lounge of laxatives – only for the elite who don’t mind the bill.
All in all, pick your fighter based on how fast you need that throne‑session.
Liam Warren
From a pharmacokinetic standpoint, Dulcolax’s bioavailability peaks within the 6‑12 hour window, delivering a robust peristaltic stimulus.
Senna’s active metabolites, sennosides A and B, undergo bacterial de‑conjugation, resulting in a comparable temporal profile but with a slightly higher variability coefficient.
Magnesium hydroxide operates via osmotic gradient formation, requiring adequate aqueous intake to achieve optimal pharmacodynamic effect.
Polyethylene glycol 3350, with its high molecular weight, creates an osmotic load that retains luminal water, yet its onset is delayed due to the need for colonic saturation.
Psyllium husk, as a soluble fiber, expands up to 10 times its weight, enhancing stool bulk and promoting transit through the graft‑type peristalsis.
Clinical decision‑making should integrate these mechanistic nuances with patient‑specific factors such as renal function, electrolyte status, and adherence potential.
Brian Koehler
Indeed, the comparative matrix presented here is quite comprehensive; however, let us not overlook the subtleties inherent in patient preference, cost‑effectiveness, and accessibility, all of which intertwine to shape therapeutic outcomes; moreover, the pharmacologic diversity ranging from stimulant to osmotic classes offers a spectrum of options that can be tailored to individual physiological responses; consequently, clinicians ought to weigh the immediacy of action against the potential for adverse events, such as abdominal cramping with Dulcolax or electrolyte shifts with magnesium, thereby fostering an informed, patient‑centric approach to constipation management.
Dominique Lemieux
While the chart does a decent job of laying out the basics, I find the glorification of stimulant laxatives like Dulcolax and Senna to be a bit overhyped, especially when we consider the long‑term repercussions of habitual use.
First, chronic stimulation can lead to colonic hyposensitivity, effectively making the gut lazy and dependent on external triggers for peristalsis.
Second, the notion that rapid onset is inherently superior fails to appreciate that many patients actually benefit more from a gentle, sustained effect that minimizes cramping and electrolyte disturbance.
Third, the osmotic agents, though slower, preserve the integrity of the intestinal mucosa and are less likely to precipitate the dreaded “laxative‑induced diarrhea” that can wreak havoc on the microbiome.
Furthermore, the cost analysis presented seems to gloss over hidden expenses; for instance, frequent purchases of cheap stimulants can cumulatively exceed the one‑time or monthly cost of a prescription‑only agent that offers a steadier, more predictable outcome.
Finally, clinicians ought to prioritize lifestyle modifications-dietary fiber, hydration, and regular physical activity-before resorting to pharmacotherapy, a principle that appears under‑emphasized in the current comparison.
In short, while Dulcolax has its place for acute relief, it should not be the default, nor should its perceived efficacy eclipse the nuanced benefits of alternative classes.
Laura MacEachern
Hey folks, just wanted to add a sunny note – if you’re looking for a gentle, budget‑friendly option, Milk of Magnesia can be a real lifesaver without the harsh cramping.
Pair it with a tall glass of water and a bit of fiber, and you’ll likely feel the difference without breaking the bank.
Remember, staying hydrated is key no matter which product you pick!
BJ Anderson
There’s a certain drama to the whole laxative selection process, isn’t there?
One moment you’re staring at a bottle of Dulcolax, hoping for a quick fix, the next you’re contemplating the slow, steady march of Psyllium for long‑term health.
It’s all about balancing urgency with comfort – you don’t want to sprint into a bathroom only to end up in a marathon of abdominal cramps.
That’s why I say keep a small stash of a fast‑acting stimulant for emergencies, but let osmotic and fiber options be your daily go‑to.
In the end, the best regimen is the one that respects both your body’s rhythm and your schedule.
Abhinav Sharma
🧐 When we weigh the pros and cons of each laxative, we enter a fascinating philosophical realm where the body’s natural rhythm meets modern pharmaceutics.
Consider Dulcolax as the swift messenger of relief, yet its urgency can sometimes feel like a storm‑like disturbance in the gut’s serenity.
Contrast that with the calm, methodical approach of polyethylene glycol, which, though slower, harmonizes with the body’s innate water balance.
💡 The choice, therefore, becomes a reflection of one’s personal philosophy: do we prioritize immediate gratification or embrace a slower, perhaps more sustainable journey?
🍃 And let’s not forget that incorporating wholesome foods and mindful hydration can serve as the most elegant adjunct to any pharmacologic plan.
Welcher Saltsman
I prefer the cheap milk of magnesia.
Alexander Rodriguez
Well, the cheap option still works if you stay consistent with water intake.
april wang
Having spent a considerable amount of time reviewing the intricacies of each listed laxative, I feel compelled to share a reflective synthesis that may aid those navigating this often uncomfortable terrain.
First, the rapid onset of stimulant agents like Dulcolax and Senna can be a double‑edged sword, offering prompt relief while simultaneously introducing the risk of abdominal cramps that may be unsettling for some individuals.
Second, osmotic laxatives such as Milk of Magnesia and polyethylene glycol provide a gentler, albeit slower, mechanism that aligns more closely with the body’s natural hydration processes, reducing the likelihood of harsh side‑effects.
Third, the bulk‑forming nature of psyllium husk cultivates a gradual improvement in stool consistency, fostering long‑term regularity without the need for pharmacologic intervention in many cases.
Moreover, the financial considerations highlighted in the comparative table cannot be dismissed; while Dulcolax and Senna are affordable, the cumulative cost of repeated purchases may rival that of a single prescription of lubiprostone for patients with chronic refractory constipation.
In practice, I recommend a tiered approach: begin with lifestyle modifications – increased fiber intake, adequate fluid consumption, and regular physical activity – before escalating to a fast‑acting stimulant for acute episodes.
Should the need for a more potent or targeted therapy arise, a clinician‑guided transition to an osmotic agent or even a prescription‑only option can be justified based on the patient’s underlying health profile and response history.
Ultimately, the goal is to harmonize efficacy, safety, and cost, empowering individuals to manage their gastrointestinal health with confidence and minimal disruption to daily life.