AERD Risk Assessment Tool
Aspirin-Exacerbated Respiratory Disease Risk Assessment
This tool helps you assess your risk of having Aspirin-Exacerbated Respiratory Disease (AERD) based on common symptoms and medical history. AERD is a condition where asthma, nasal polyps, and NSAID sensitivity occur together. This assessment is not a diagnosis but can help you discuss concerns with your healthcare provider.
When you take a simple painkiller like ibuprofen or aspirin, most people feel better. But for some, it triggers something dangerous: wheezing, nasal congestion, and even trouble breathing. This isn’t just an allergy. It’s a condition called Aspirin-Exacerbated Respiratory Disease (a chronic condition where asthma, nasal polyps, and NSAID sensitivity occur together), or AERD. It’s often called Samter’s Triad, named after the doctor who first described it in the 1960s. If you have asthma and nasal polyps - especially if you’ve had them for years - and you react badly to pain relievers, this might be what’s going on.
What Exactly Is AERD?
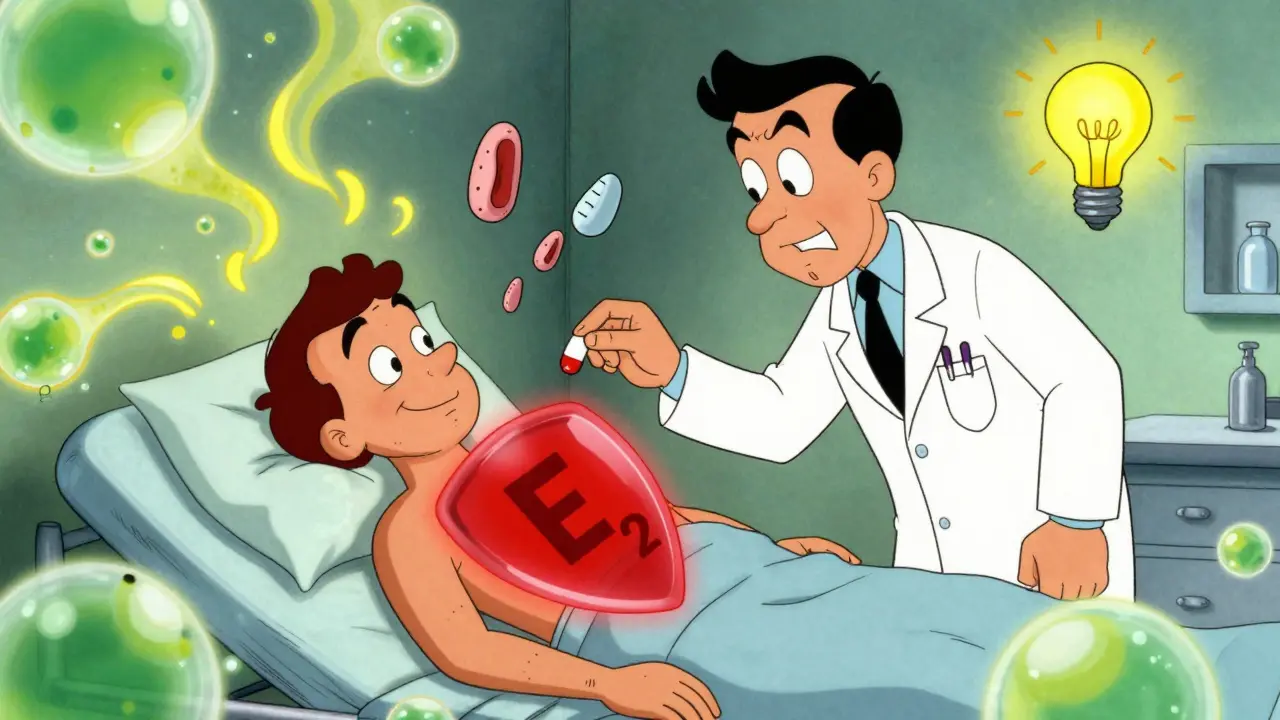
AERD isn’t an allergy in the traditional sense. You’re not allergic to aspirin the way someone might be allergic to peanuts. Instead, your body’s immune system is already in overdrive because of chronic inflammation in your airways and sinuses. When you take a drug that blocks COX-1 - like aspirin, ibuprofen, or naproxen - it throws your body’s chemistry out of balance. Your cells start producing too much of certain inflammatory chemicals (like leukotrienes) and not enough of protective ones (like prostaglandin E2). The result? Severe swelling in your nose, lungs, and sinuses.
This condition almost always shows up in adults between 20 and 50. It doesn’t run in families. You don’t inherit it. It just… happens. And once it starts, it doesn’t go away. The three key signs are:
- Chronic asthma that’s hard to control
- Recurring nasal polyps (growths in the nose that block airflow)
- Severe reactions to aspirin or other NSAIDs
It’s not rare. About 9% of all adults with asthma have AERD. If you have both asthma and nasal polyps? That number jumps to 30%. Yet, most doctors miss it. Patients wait an average of 7 to 10 years before getting the right diagnosis.
How It Feels: Symptoms You Can’t Ignore
If you have AERD, your daily life looks different. You’re not just dealing with occasional congestion. You’re living with constant stuffiness, a loss of smell, and frequent sinus infections. More than 90% of people with AERD lose at least part of their sense of smell. That’s not just inconvenient - it affects your appetite, your safety (can you smell smoke or gas?), and even your mood.
Your asthma? It’s worse than average. You’re more likely to need emergency care. Studies show AERD patients visit the ER 2.3 times more often than other asthma patients. Hospital stays are 1.8 times more frequent. Standard inhalers work poorly - only about 35% of patients get good control with them alone.
Then there’s the NSAID trigger. Take a single Advil or Aleve? Within 30 to 120 minutes, you’ll likely feel:
- Intense nasal congestion
- Frontal headache or sinus pressure
- Red, watery eyes
- Wheezing and chest tightness
And here’s the part most people don’t know: alcohol makes it worse. About 75% of AERD patients react to alcohol - even one glass of wine or beer. It’s not the alcohol itself. It’s how it interacts with your inflamed airways. You might get flushed, nauseous, or have a sudden asthma attack after just a sip.
Why Standard Treatments Often Fail
Most asthma patients do well with inhalers. Steroids. Bronchodilators. But AERD? It’s a different beast. The inflammation here is deeper, more stubborn. It’s not just about tightening airways - it’s about your entire respiratory system being stuck in high-alert mode.
Surgery to remove nasal polyps? It’s common. But in AERD patients, polyps grow back faster - often within 6 months. In non-AERD patients, recurrence is around 30-40% in 18 months. For AERD? It’s 70-100%. That means multiple surgeries, repeated recovery periods, and ongoing costs.
Biologics like dupilumab (Dupixent) help. They target specific immune signals (IL-4 and IL-13) that drive AERD inflammation. Studies show they reduce polyp size by 50-60%. But they cost $38,500 a year. Only 38% of patients have insurance that covers them. And they don’t fix the NSAID sensitivity.
The Game-Changer: Aspirin Desensitization
There’s one treatment that doesn’t just manage symptoms - it changes the disease course. It’s called aspirin desensitization.
Here’s how it works: In a controlled hospital setting, you’re given tiny, increasing doses of aspirin over 2-3 days. Under medical supervision, you’re monitored for reactions. If you tolerate the full dose (usually 650 mg twice daily), your body learns to handle it. Your inflammation drops. Your nasal polyps shrink. Your asthma improves. Your sense of smell often comes back.
Studies show 85% of patients who complete the process see major improvement. Sinus surgery rates drop by 60%. Emergency visits fall. Quality of life jumps. A 2022 survey of over 1,200 AERD patients found 68% reported big improvements after desensitization.
But here’s the catch: Only 12% of allergy clinics in the U.S. offer this. You need to find a specialist. There are only about 35 dedicated AERD centers nationwide. And you have to commit to taking daily aspirin forever. No skipping days. No switching to ibuprofen. If you stop, your symptoms return within weeks.
Why So Many People Stay Undiagnosed
Most patients don’t connect their reactions to NSAIDs with their asthma and polyps. They think, “I’m allergic to Advil.” They avoid painkillers. They get sinus surgery. They feel better for a while. Then the polyps come back. And again. And again.
One Reddit user, ‘PolypWarrior87’, wrote: “It took me 11 years and 4 ENT specialists before someone finally connected my asthma attacks after taking Advil to my nasal polyps.” That’s not unusual.
Doctors often miss the alcohol link. Or they assume nasal polyps in adults are just “sinus trouble.” They don’t ask about NSAID reactions. And when patients avoid aspirin, they’re not told why - or what else might help.
There’s also fear. The idea of being given aspirin while you’re wheezing sounds terrifying. But under proper medical care, the risk is low. The success rate is 92% at top centers. And the long-term benefits? Life-changing.
What You Can Do Right Now
If you have asthma and nasal polyps - and you’ve ever had a bad reaction to ibuprofen, aspirin, or alcohol - you need to get tested. Here’s how to start:
- Stop assuming your NSAID reactions are “just allergies.” Write down every time you had a reaction - what you took, what happened, how long it lasted.
- Find an allergist who specializes in AERD. Use the Samter’s Society website to locate a center near you.
- Ask about aspirin challenge testing. It’s not dangerous if done right.
- If you’re a candidate, ask about desensitization. It’s not a cure, but it’s the closest thing we have.
- Keep a log of your symptoms, especially after alcohol or NSAID exposure. Bring it to your appointment.
You don’t have to live with constant congestion, lost smell, and fear of painkillers. This condition is treatable. But you have to know what you’re dealing with.
The Bigger Picture
AERD affects about 1.2 million Americans. It costs the healthcare system $1.8 billion a year - mostly from repeated surgeries and ER visits. But it’s not just a medical issue. It’s a quality-of-life issue. Losing your sense of smell. Being afraid to take a pain reliever. Having to plan your life around what you can and can’t eat or drink.
Research is moving fast. A new drug, MN-001, showed 70% reduction in polyp recurrence in early trials. A national registry is now tracking 2,000 patients to find better treatments. By 2028, experts predict precision medicine will cut surgery rates by 40%.
But until then, the best tool we have is awareness. And action. If you suspect you have AERD, don’t wait. Don’t assume it’s just “bad asthma.” Get tested. Ask the right questions. And know that there’s a path forward - even if it’s not simple.
Can you outgrow Aspirin-Exacerbated Respiratory Disease?
No. AERD is a lifelong condition. It doesn’t go away on its own. Even if your symptoms seem mild, the underlying inflammation remains. Avoiding NSAIDs helps prevent reactions, but it doesn’t stop the disease from progressing. The only treatment that alters the disease course is aspirin desensitization - and even then, you must continue daily aspirin to maintain the benefit.
Are all NSAIDs dangerous for AERD patients?
Most are. Any NSAID that blocks COX-1 - like aspirin, ibuprofen, naproxen, diclofenac, and ketoprofen - can trigger a reaction. But not all pain relievers are the same. Acetaminophen (Tylenol) is generally safe because it doesn’t strongly inhibit COX-1. Some newer NSAIDs like celecoxib (Celebrex) may be tolerated, but only under doctor supervision. Never assume a painkiller is safe without checking with your specialist.
Why does alcohol trigger reactions in AERD?
Alcohol doesn’t directly cause the reaction. It worsens the inflammation already present in your airways. It increases blood flow to your nasal passages and sinuses, which makes swelling worse. It may also interfere with how your body processes inflammatory chemicals. About 75% of AERD patients react to alcohol - sometimes after just one drink. Wine, beer, and liquor can all trigger symptoms. The reaction isn’t about sugar or sulfites - it’s about how your body handles the alcohol when you have AERD.
Is AERD the same as a food allergy?
No. AERD is not an IgE-mediated allergy like peanut or shellfish allergies. You won’t test positive on skin prick or blood tests for NSAID allergy. It’s a pharmacological intolerance - meaning it’s caused by how your body reacts to a drug’s effect on your immune system. It’s more like a metabolic malfunction than an allergic response. That’s why traditional allergy treatments (like epinephrine) don’t work for AERD reactions.
Can children get AERD?
Almost never. AERD is an adult-onset condition. It rarely starts before age 20. If a child has asthma and nasal polyps, it’s likely a different condition - like cystic fibrosis, primary ciliary dyskinesia, or a genetic immune disorder. AERD is almost exclusively seen in adults, especially those who developed asthma later in life.
What happens if I stop taking aspirin after desensitization?
Your symptoms will return - usually within 2 to 4 weeks. The benefits of desensitization depend on daily aspirin use. It’s not a one-time fix. You must take 650 mg twice a day, every day, to keep the inflammation under control. Skipping doses or switching to other NSAIDs will undo the progress. Think of it like taking blood pressure medication - if you stop, your condition comes back.






