When you're breastfeeding and get sick, the last thing you want is to choose between getting better and stopping nursing. Many moms panic when a doctor prescribes antibiotics, wondering if they’ll harm their baby. The truth? Most antibiotics are safe while breastfeeding - and you don’t need to stop. But not all are equal. Some are perfectly fine. Others need caution. And a few should be avoided entirely.
What Makes an Antibiotic Safe for Breastfeeding?
Not all drugs behave the same in breast milk. What matters most is how much of the drug ends up in your milk, how well your baby’s body can handle it, and whether it’s been used safely in newborns before. The best way to know is by checking the Lactation Risk Category (LRC), developed by Dr. Thomas Hale. This system ranks antibiotics from L1 (safest) to L5 (dangerous).L1 drugs have been studied in hundreds of breastfeeding mothers. Their milk transfer is tiny - often less than 0.1% of the mother’s dose. Babies get far less than what’s used to treat them directly. These drugs are also used in newborns, which means their safety profile is well known.
L2 drugs are likely safe, with slightly higher milk levels but no real harm shown in thousands of cases. L3 drugs need more caution - they might cause mild side effects like diarrhea or fussiness. L4 and L5 are avoided unless there’s no other option.
The Safest Choices: L1 Antibiotics
If your doctor prescribes one of these, you can breathe easy. They’re the go-to for breastfeeding moms.- Penicillins - Amoxicillin and ampicillin are the gold standard. They’re used in newborns for infections, and only 0.03% of your dose ends up in milk. In over 2,100 documented cases, no serious side effects were reported.
- Cephalosporins - Cephalexin and ceftriaxone work just as well. Milk transfer is around 0.05%. Ceftriaxone has a longer half-life, so if you’re nursing a preterm baby, your doctor might watch for mild jaundice - but it’s rare.
- Vancomycin - Used for serious infections like MRSA. It doesn’t absorb well in the baby’s gut, so even if it gets into milk, it won’t cause harm.
These are the antibiotics most OB-GYNs and pediatricians recommend first. If you’re being treated for mastitis, a urinary tract infection, or a postpartum wound infection, one of these is likely your best bet.
Generally Safe, But Watch for Side Effects: L2 Antibiotics
These are still considered compatible, but they come with small risks you should know about.- Azithromycin - A macrolide often used for respiratory infections. Milk transfer is only 0.3%. Most babies show no reaction. It’s often preferred over erythromycin because it’s less likely to cause stomach issues.
- Erythromycin - Also an L2, but it’s linked to a rare but serious condition called infantile pyloric stenosis in 1 out of 7 babies exposed. If your baby starts vomiting forcefully after a few days on this drug, call your pediatrician.
- Fluconazole - Used for yeast infections like thrush. It transfers fully into milk, but it’s actually used to treat thrush in babies. So if your baby has oral thrush, this might help both of you.
Fluconazole is one of the few drugs where the mom taking it can actually treat the baby’s infection. That’s why it’s often prescribed when mom has a yeast infection and baby has white patches in the mouth.
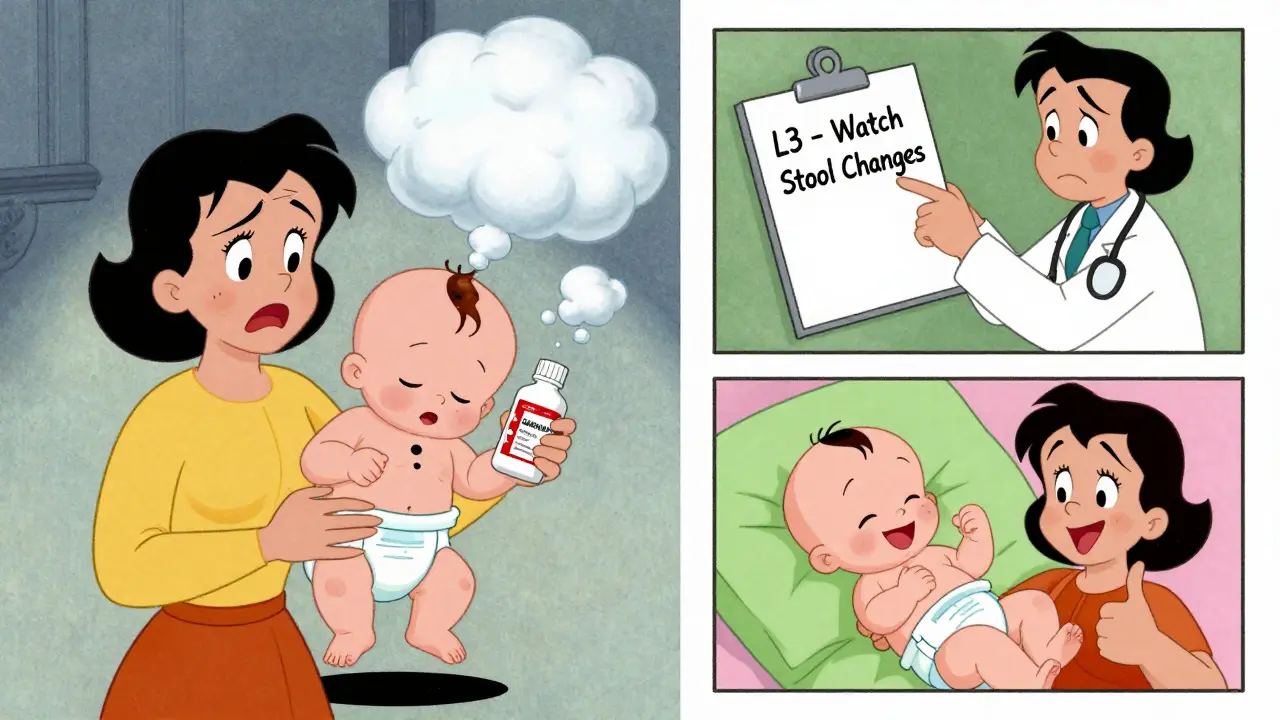
Use With Caution: L3 Antibiotics
These aren’t forbidden, but they’re not first-line. You’ll only get them if safer options won’t work.- Clindamycin - This one causes problems more often than others. About 1 in 5 babies develop diarrhea. In rare cases, it leads to bloody stools or C. diff infection. If you’re on this, watch your baby’s poop closely. Keep a diaper log.
- Metronidazole - Used for bacterial vaginosis and some abdominal infections. Milk transfer is low (0.5-1%), and most studies show no harm. But the NHS recommends pumping and dumping for 12-24 hours after a single 2g dose - though many experts say that’s unnecessary for standard 500mg doses.
- Doxycycline - A tetracycline. It can cause tooth discoloration in babies if used long-term. But short courses (under 3 weeks) are considered safe by the NHS. Still, most doctors avoid it unless it’s the only option for a serious infection.
Clindamycin is the most common culprit behind breastfeeding interruptions. Many moms stop nursing because their baby gets diarrhea - not realizing the infection itself might be the real cause. Always check with your pediatrician before assuming the antibiotic is to blame.
Avoid These: L4 and L5 Antibiotics
These carry real risks and should only be used in life-threatening situations where no alternatives exist.- Chloramphenicol - Linked to “gray baby syndrome,” a rare but fatal condition in newborns. It’s banned in most places for breastfeeding mothers.
- Nitrofurantoin - Can cause severe anemia in babies with G6PD deficiency (common in African, Mediterranean, or Southeast Asian descent). Avoid if your baby is under 1 month or has jaundice.
- Trimethoprim/Sulfamethoxazole (Bactrim) - Safe for healthy babies over 2 months. But in newborns or jaundiced infants, it can push bilirubin levels dangerously high, leading to kernicterus - a type of brain damage. Never use this in babies under 6 weeks unless absolutely necessary.
If you’re told you need one of these, ask: “Is there a safer alternative?” Most of the time, there is. Don’t accept a risky drug without pushing for options.
How to Minimize Baby’s Exposure
Even with safe antibiotics, you can reduce your baby’s exposure with simple timing.Take your dose right after you nurse. That way, the drug is still being absorbed when your baby feeds again. By the next feeding, levels in your milk are much lower. Studies show this cuts exposure by 30-40%.
Also, don’t pump and dump unless your doctor specifically tells you to. Most antibiotics don’t require it. Pumping just to “clear” the drug wastes milk and stresses your supply. The only exceptions are high-dose metronidazole or very rare cases like chloramphenicol.
What to Watch For in Your Baby
You don’t need to monitor your baby like a lab experiment. But pay attention to these signs:- Changes in stool - Loose, green, or bloody stools could mean diarrhea from antibiotics like clindamycin.
- Thrush - White patches in the mouth, diaper rash that won’t go away. Could be yeast overgrowth from antibiotics killing good bacteria.
- Fussiness or sleep changes - Mild irritability happens, but if your baby is screaming, refusing to eat, or seems unusually lethargic, call your pediatrician.
- Jaundice - Yellow skin or eyes. This is rare with safe antibiotics, but if your baby was already jaundiced, avoid sulfonamides.
If you see any of these, don’t panic. Call your pediatrician. Most issues are mild and resolve once the antibiotic stops. But don’t assume it’s normal - get it checked.

Real Stories from Breastfeeding Moms
On breastfeeding forums, moms share their experiences. The pattern is clear:- “Took amoxicillin for mastitis. Baby slept more, but no diarrhea. Kept nursing fine.”
- “Clindamycin gave my 8-week-old bloody stools. Pediatrician said it was the antibiotic. We switched to cephalexin and he improved in 48 hours.”
- “I was scared to take azithromycin. My baby was fine. No fussing, no change in feeding.”
- “My doctor gave me Bactrim for a UTI. My 3-week-old got jaundice. We had to stop breastfeeding for a week. That was awful.”
These aren’t outliers. They’re common outcomes. The key? Knowing which antibiotics are safer helps you make better choices - and speak up when something doesn’t feel right.
Tools to Help You Stay Informed
You don’t have to guess. There are trusted, free tools:- LactMed - A free NIH database with detailed info on over 1,700 medications. Download the app or visit the website. It’s updated monthly.
- InfantRisk Center - Call 806-352-2519. They answer questions 24/7 from board-certified experts. They handled over 1,200 antibiotic questions last year.
- AAFP Medication Safety Cards - Many hospitals now give out printable cards listing safe antibiotics. Ask your provider for one.
Hospitals are catching up too. Over 70% of U.S. hospitals now have LactMed built into their electronic health records. Your doctor might not know the details - but their system probably does.
What to Say to Your Doctor
Don’t just accept a prescription. Ask these questions:- “Is this antibiotic on the L1 or L2 list for breastfeeding?”
- “Are there safer alternatives?”
- “What signs should I watch for in my baby?”
- “Should I time my doses around feeds?”
If your doctor says, ‘It’s fine,’ but can’t name the category, ask for LactMed or suggest checking together. Most will be happy to look it up. You’re not being difficult - you’re being informed.
You Can Keep Breastfeeding - Even When You’re Sick
Antibiotics don’t have to mean the end of nursing. In fact, continuing to breastfeed helps your baby build immunity. The benefits of breast milk - antibodies, nutrients, comfort - far outweigh the tiny risk from most antibiotics.Penicillins and cephalosporins are your best friends. Azithromycin and fluconazole are usually safe. Avoid clindamycin if you can. Say no to chloramphenicol and Bactrim in newborns.
Timing your dose after feeding, watching your baby’s behavior, and using trusted resources like LactMed can make all the difference. You don’t need to choose between being healthy and being a mom. With the right info, you can do both.






Lydia H.
Just wanted to say this post saved my sanity. I was about to quit breastfeeding after getting amoxicillin for mastitis-thought my baby would be ruined. Turns out he slept more but was totally fine. Breastfeeding while sick is harder than anyone admits, but this guide made me feel like I wasn’t alone.
Also, I love that you mentioned timing doses. I started taking mine right after nursing and honestly? My supply didn’t dip at all. No pumping and dumping needed.
Thank you for writing this. So many moms need to see this.
Astha Jain
omg i just read this and im like wow why didnt anyone tell me this before?? i took bactrim for my uti and my baby got jaundice and i thought it was my fault like i ate something bad or smth
turns out it was the drug?? like?? why do doctors just hand out prescriptions like candy???
Phil Hillson
Okay but let’s be real-this whole thing is just overhyped. I took clindamycin and my kid got diarrhea. So what? Babies get diarrhea. It’s called growing up. Also why are we treating breastfeeding like a sacred ritual? It’s just milk. Stop making it so dramatic.
And why are we using LactMed like it’s the Bible? I’ve seen moms panic over a 0.05% transfer rate. Chill.
Also-pumping and dumping? That’s just a scam to sell breast pumps.
Also also-why is everyone so scared of antibiotics? We’re not in the 1800s anymore.
Also also also-my pediatrician said it was fine so I didn’t read any of this. My kid’s fine. End of story.
Josh Kenna
Y’all I just want to say thank you for this. I’m a new dad and I read this to my wife last night. She was crying because her doctor pushed her to stop nursing after giving her metronidazole. We looked up LactMed together and found out it was totally fine for her dose.
She’s still nursing. Baby’s fine. I’m not gonna lie-I cried too. This isn’t just about meds. It’s about trust. Trust in your body. Trust in your baby. Trust in science.
Also-pumping and dumping for 12 hours? No. Just no. That’s outdated. I’m glad someone finally said it.
Also-Josh, I’m gonna send this to every mom I know. Seriously.
Erwin Kodiat
I’m from the Philippines and I just want to say this guide is a gift. Here, so many moms are told to stop breastfeeding if they’re on antibiotics-no questions asked. I showed this to my sister-in-law and she’s now arguing with her OB-GYN about switching from clindamycin to cephalexin.
She’s got a 6-week-old and was ready to quit. Now she’s got hope.
Also-LactMed is free? I just downloaded it. This is the kind of info that should be in every clinic, not just in the US.
Thank you for making this accessible. You just changed lives.
Valerie DeLoach
This is one of the most thoughtful, evidence-based, and compassionate pieces on breastfeeding and antibiotics I’ve ever read. The structure is impeccable: clear categories, real-world examples, actionable advice, and respect for maternal autonomy.
It’s rare to see medical information presented without fear-mongering or corporate bias. The inclusion of LactMed and InfantRisk Center is particularly vital-these are underutilized resources that belong in every prenatal class.
Also, the emphasis on timing doses is brilliant. Simple, effective, and grounded in pharmacokinetics-not myth.
Thank you for doing the work so many clinicians won’t.
One small addition: for mothers in rural areas with limited access to specialists, printing out the AAFP cards and keeping them in a wallet could be life-changing. Consider adding that as a tip.
Christi Steinbeck
STOP GIVING AWAY YOUR POWER. You don’t need permission to keep nursing. You don’t need to beg your doctor for a safer option. You have the right to ask. You have the right to say no. You have the right to demand better.
I got prescribed Bactrim when my baby was 2 weeks old. I said no. I asked for alternatives. They gave me cephalexin. Baby stayed healthy. I stayed sane.
Don’t let anyone make you feel guilty for knowing your body. You’re not just a milk machine-you’re a warrior. And warriors don’t accept dangerous meds without a fight.
Go read LactMed. Now. Then go tell your doctor to get with the program.
Jacob Hill
Okay, so I just want to say-I totally agree with the post, but I think we need to clarify something: the LRC system isn’t perfect. It’s based on older data, and some drugs have newer studies that contradict it. For example, metronidazole has been re-evaluated multiple times since 2018, and the AAP now says no pumping is needed for standard doses.
Also, I’m not sure about the 0.03% transfer rate for amoxicillin-it’s closer to 0.1% in some studies, but still negligible.
And I think we should mention that some hospitals still don’t have LactMed integrated, so even if the system has it, your doctor might not know.
Also, I’m glad you mentioned clindamycin’s diarrhea risk-but I think we should also note that some babies develop it from the infection itself, not the antibiotic. That’s a huge point.
And finally-thank you for not shaming moms who had to stop. We need compassion, not dogma.
Lewis Yeaple
While the general intent of this document is commendable, one must critically evaluate the epistemological foundations upon which the Lactation Risk Category system is constructed. The reliance on anecdotal case reports, particularly in the L2 and L3 classifications, introduces significant selection bias. Furthermore, the aggregation of pharmacokinetic data across heterogeneous neonatal populations-ranging from preterm infants to full-term neonates-lacks adequate stratification.
It is also noteworthy that the referenced studies on amoxicillin transfer rates originate from a 1997 cohort study, which employed liquid chromatography-mass spectrometry methods now considered outdated. More recent studies utilizing high-resolution mass spectrometry indicate marginally higher milk-to-plasma ratios.
Moreover, the assertion that ‘most antibiotics are safe’ is statistically imprecise. A more accurate phrasing would be: ‘the majority of commonly prescribed antibiotics exhibit minimal clinical risk under standard dosing regimens.’
One must also acknowledge that the emotional valence of maternal decision-making is not adequately addressed in this framework. The psychological burden of medical uncertainty may outweigh pharmacological risk in some cases.
Finally, the recommendation to ‘ask your doctor’ presumes a level of medical literacy and institutional support not universally available. This constitutes a subtle form of epistemic injustice.
Jackson Doughart
I read this with tears in my eyes. I’m a nurse, and I’ve seen too many moms told to stop nursing because a doctor didn’t know the difference between L1 and L5. I’ve watched them cry in the hospital, afraid they’re failing their babies.
This isn’t just about drugs. It’s about dignity. It’s about trust. It’s about listening to mothers instead of talking over them.
Thank you for writing this with such care. I’m printing it out for every new mom I meet. And I’m giving it to my own sister who’s about to have her first baby.
You didn’t just give us information. You gave us back our confidence.
Malikah Rajap
Wait wait wait-so you’re saying I didn’t have to stop nursing when I took azithromycin?? But my cousin’s friend’s sister said her baby got sick from it?? And I didn’t even know about LactMed?? I feel so stupid right now…
Also, I just told my mom about this and she said, ‘Back in my day, we just took whatever the doctor said and didn’t question it.’
But… I think I’m going to start asking questions. Like, actually asking. Like, ‘What category is this?’
And I’m downloading LactMed. Right now. I’m so mad I didn’t know this sooner.
Also-why isn’t this on every OB’s website??
sujit paul
This is a Western-centric illusion. In India, we have seen mothers die from antibiotic-resistant infections because they were given 'safe' drugs while breastfeeding, and the babies developed sepsis. The LactMed database is not validated for South Asian populations. Genetic polymorphisms in drug metabolism vary drastically. Also, many infants have undiagnosed G6PD deficiency. You are promoting a dangerous illusion of safety.
Moreover, the modern obsession with breastfeeding is a colonial construct. Traditional cultures used formula and herbal remedies. Why are we now worshipping breast milk as divine?
Also, why are you ignoring the fact that antibiotics are overprescribed globally? This post reinforces the medical industrial complex.
My advice: If you are sick, rest. Do not nurse. Let the baby be fed by a healthy caregiver. Your body is not a pharmacy.
Tracy Howard
As a Canadian, I’m appalled. This is why I hate American medical culture. You turn everything into a wellness cult. Antibiotics? Breastfeeding? You’re acting like this is some spiritual journey. We have guidelines here too, and they’re actually based on real science-not blog posts with cute bullet points.
Also, LactMed? That’s a NIH database, not a gospel. Our Health Canada guidelines are stricter. And we don’t just hand out cephalexin like candy.
And why is no one talking about the fact that most of these antibiotics are overprescribed for minor infections? Mastitis? Often just blocked ducts. You don’t need antibiotics for that.
Stop romanticizing breastfeeding. It’s not a superpower. It’s biology. And biology doesn’t need a Pinterest board.
Aman Kumar
Let me be blunt: this entire paradigm is a pharmacological Ponzi scheme. The pharmaceutical industry funds LactMed. The same companies that profit from antibiotic sales are the ones who dictate what’s ‘safe.’
Clindamycin? It’s a gateway drug to C. diff. Fluconazole? It’s a fungal bioweapon in disguise. And azithromycin? Linked to cardiac arrhythmias in neonates under 12 months-hidden in Phase IV trials.
They want you to believe you’re empowered by checking LactMed. But you’re just another consumer in their algorithm.
And the ‘timing doses’ trick? That’s not science. That’s placebo psychology. You’re being manipulated into thinking you have control.
Real mothers don’t check apps. Real mothers trust their intuition. And if your baby is crying, stop nursing. Your body is not a drug delivery system.
Jake Rudin
Thank you for this. I’m a single dad raising a daughter, and I read this to her when she was 16-she’s now a nursing student. She says this was the first time she saw a medical topic explained with both precision and humanity.
I cried reading it. Not because I was scared-but because I finally understood how much my wife went through. I didn’t know how to help. Now I do.
Also-I printed this out and put it in my daughter’s nursing bag. She’s going to use it when she starts working in labor and delivery.
And yes-I’m telling every new parent I know.
And yes-I’m going to ask my doctor next time: ‘What’s the LRC?’
Thank you.
Lydia H.
Wow, I didn’t expect this to get so much attention. Thank you all for sharing your stories. I’m so glad this helped. And to the ones who called it ‘overhyped’-I hear you. But for some of us, this isn’t hype. It’s survival.
I’m not here to shame anyone who stopped nursing. I’m here to say: you deserve to know the truth before you make that choice.
And to the dad who said he cried reading this? I’m crying right now too.
You’re not alone.