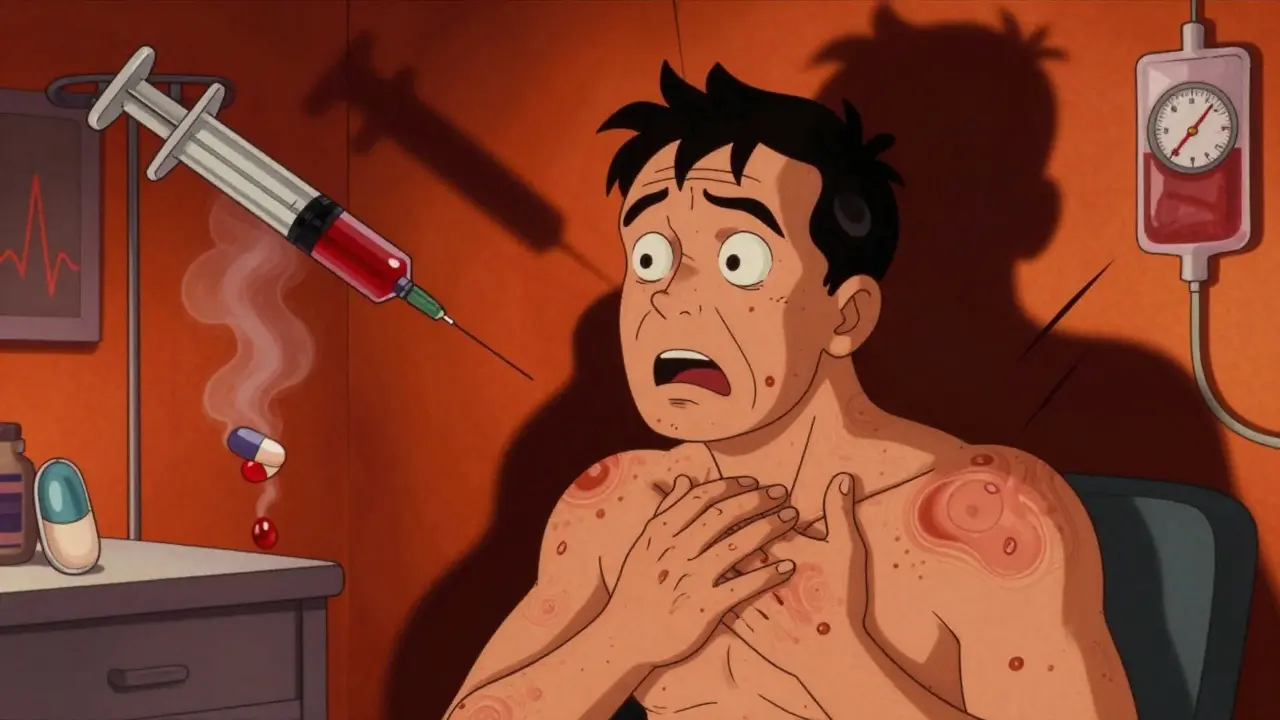
What anaphylaxis really looks like when it’s triggered by a medication
It starts fast. One moment you’re fine. The next, your throat feels tight, your skin breaks out in hives, and your chest feels like it’s being squeezed. Your blood pressure drops. You can’t catch your breath. This isn’t anxiety. It’s not a panic attack. It’s anaphylaxis - a full-body, life-threatening allergic reaction to a medication. And if you don’t act fast, it can kill you.
Medications are one of the top triggers for anaphylaxis in hospitals and clinics. Antibiotics like penicillin, painkillers like ibuprofen, chemotherapy drugs, and even IV contrast dyes can set it off. In fact, medication-induced anaphylaxis accounts for nearly one in six of all cases. The scary part? Many of these reactions are missed at first. Doctors mistake them for side effects, infections, or even stress. But the clock is ticking - every minute counts.
The signs you can’t afford to ignore
Anaphylaxis doesn’t always start with a rash. Sometimes it starts with a feeling - like something’s wrong. Here’s what to watch for, especially if you’ve just taken a new medication:
- Sudden swelling of the lips, tongue, or throat
- Hives, itching, or flushing of the skin
- Wheezing, shortness of breath, or feeling like you’re suffocating
- Dizziness, lightheadedness, or fainting
- Nausea, vomiting, or abdominal cramps
- Rapid or weak pulse
You don’t need all of these to be in danger. The American Academy of Allergy, Asthma & Immunology says if you have any one of these three, you’re likely having anaphylaxis:
- Skin symptoms (like hives) + trouble breathing or low blood pressure
- Two or more body systems reacting (skin + gut, or skin + lungs)
- Low blood pressure after exposure to a known drug trigger
For example, a patient gets an IV antibiotic and within 10 minutes starts breaking out in hives and feels dizzy. That’s enough. Don’t wait for the swelling. Don’t wait for vomiting. If it’s sudden, it’s serious.
Why medications are especially dangerous triggers
Not all anaphylaxis is the same. Food reactions often start with itching and stomach pain. But drug reactions? They hit harder, faster, and more often involve your heart and lungs.
According to a 2023 analysis of over 12,000 cases, medication-induced anaphylaxis causes low blood pressure in nearly 60% of cases - compared to just 40% for food triggers. It also causes breathing problems in 71% of cases, versus 54% for food. And here’s the worst part: the death rate is nearly three times higher.
Why? Because in a hospital, symptoms get misread. A drop in blood pressure after surgery? Maybe it’s anesthesia. A rash after chemotherapy? Maybe it’s a side effect. A wheeze during an IV drip? Maybe it’s bronchitis. But if you’re not thinking anaphylaxis, you’re not giving epinephrine - and that’s where people die.
Studies show that in 78% of fatal cases, epinephrine was given too late - or not at all. That’s not a failure of medicine. It’s a failure to recognize.

Epinephrine: The only thing that saves lives
There is no other treatment that works like epinephrine. Antihistamines? They help with itching. Steroids? They prevent a second wave. But only epinephrine stops the runaway reaction in your body.
It works by tightening blood vessels, opening airways, and boosting heart function - reversing the collapse happening inside you. And it has to be given fast. The window is 5 to 15 minutes after symptoms start. After 30 minutes, your risk of dying jumps by 300%.
How to give it right:
- Use an auto-injector (like EpiPen or Auvi-Q)
- Inject into the outer thigh - through clothing if needed
- Hold for 3 seconds
- Call 911 even if you feel better
Doctors at Johns Hopkins found that when staff were trained with simulation drills, epinephrine use in emergencies jumped from 48% to 90% in six months. That’s not magic. That’s practice.
And here’s the truth: if you’ve ever had anaphylaxis from a drug, you should carry an auto-injector. But only 47% of patients get one prescribed after their first episode. That’s unacceptable.
What doctors get wrong - and how to protect yourself
Many reactions are mistaken for other things:
- Red man syndrome from vancomycin (a common antibiotic): Red skin, itching, flushing - looks like anaphylaxis, but no drop in blood pressure or breathing trouble. It’s not life-threatening, but it’s often treated like it is.
- Panic attacks: Fast heartbeat, dizziness, tingling - sounds similar, but no swelling or wheezing.
- Sepsis: Fever, low BP, confusion - can mimic anaphylaxis, but develops over hours, not minutes.
One ER nurse in Boston told me about a patient who got IV contrast and collapsed. The team thought it was a vasovagal faint. They gave fluids. They waited. It wasn’t until the patient started wheezing and her oxygen dropped to 82% that someone said: “This is anaphylaxis.” Epinephrine was given. She recovered. But it took 18 minutes - too long.
Here’s what you can do:
- Know your drug allergies. Write them down. Keep them on your phone.
- Ask: “Is this medication known to cause allergic reactions?”
- Speak up if you feel weird. Don’t say “I’m fine.” Say “I feel like something’s wrong.”
- After any reaction, get a referral to an allergist. You need testing to know what’s safe.

What’s changing - and what you need to know now
The medical world is waking up. In 2023, the FDA required stronger warning labels on all biologic drugs - things like cancer treatments and autoimmune therapies. Hospitals are being forced to have anaphylaxis protocols by law, starting January 2024.
There’s also new tech. A rapid blood test called AllergoCheck can now confirm penicillin allergy in 15 minutes. That’s huge. For years, people were told they were allergic to penicillin based on a childhood rash - but 90% of them weren’t. Now we can test and free them from unnecessary drug restrictions.
But here’s the catch: none of this matters if you don’t know the signs. Even the best test won’t help if the nurse doesn’t recognize the symptoms. And even the fastest auto-injector won’t save you if it’s locked in a cabinet.
The real solution? Education. For patients. For doctors. For nurses. For paramedics.
What to do after an anaphylactic reaction
If you’ve had one, you’re at higher risk for another. Here’s your checklist:
- Get an epinephrine auto-injector - and carry it everywhere.
- See an allergist within 2 weeks. They’ll do skin or blood tests to confirm what caused it.
- Get a medical alert bracelet. It should say: “Anaphylaxis to [drug name].”
- Teach a family member or friend how to use your injector.
- Update your electronic medical records. Make sure every doctor you see knows.
- Keep a written record: What drug? When? What happened? How was it treated?
And if you’re ever unsure - give the epinephrine. It’s safe. Even if you’re wrong, it won’t hurt you. But if you wait, it could kill you.
Final truth: You’re not overreacting
If you’ve ever felt a strange tightness after a shot or pill - and you thought, “Maybe I’m being dramatic” - you weren’t. You were smart.
Anaphylaxis doesn’t care if you’re young, healthy, or have never had allergies before. It doesn’t care if the drug was prescribed by a top doctor. It doesn’t care if you’ve taken it before without issue. One time is enough.
The system isn’t perfect. Mistakes happen. But you can control your response. Know the signs. Carry the injector. Speak up. Save your life.






Nancy Kou
I had a reaction to penicillin in college and thought it was just a bad rash. Turns out I was seconds from anaphylaxis. Now I carry two EpiPens everywhere. Don't wait until it's too late. This post saved my life.
Hussien SLeiman
I'm not convinced this is as common as they say. I've been a nurse for 22 years and in all that time, I've seen maybe three true anaphylactic reactions from meds. The rest are just anxiety, vasovagal episodes, or people overreacting to minor side effects. We've turned every little itch into a crisis. Epinephrine isn't candy. It's a powerful drug that should be reserved for true emergencies, not people who feel 'a little weird' after a pill.
Frank Drewery
This is so important. I'm a paramedic and I've seen too many cases where epinephrine was delayed because everyone was second-guessing. That 5-minute window is everything. I wish every patient got a copy of this when they left the ER. Knowledge saves lives.
Danielle Stewart
If you've ever had even a mild reaction, please get tested. I used to think I was allergic to NSAIDs because I got a rash once. Turns out it was a viral infection. Allergist confirmed I'm fine. Now I take ibuprofen without fear. Don't assume. Get tested.
mary lizardo
The article contains several grammatical inconsistencies and an overreliance on emotionally charged language designed to provoke fear rather than inform. For instance, the phrase 'it can kill you' is hyperbolic and unscientific. Furthermore, the assertion that 'one time is enough' lacks empirical grounding in immunological literature. The FDA's new labeling requirements are prudent, but the conflation of non-life-threatening reactions with anaphylaxis is medically irresponsible.
jessica .
This is all part of the Big Pharma agenda. They want you scared so you'll buy epinephrine pens instead of just taking a pill. And don't get me started on the 'medical alert bracelet' nonsense. That's just another way for them to track you. I don't trust hospitals. I don't trust drugs. I don't trust this post. It's all a scam.
Ryan van Leent
Ive had 3 reactions and never needed epinephrine. Why are they pushing this so hard. People are getting scared over nothing. I took amoxicillin 5 times before I got a rash. I stopped taking it. Done. No big deal. Why do we need all this drama
Sajith Shams
You're all missing the point. In India, we don't have access to EpiPens. We don't even have proper allergy testing. The real issue is systemic neglect. If you're in a developed country and you're not carrying an auto-injector after a reaction, you're negligent. But in places like mine, the problem isn't awareness-it's access. Stop preaching to the choir and fix the infrastructure first.
Adrienne Dagg
I'm so glad this exists 😭 I had a reaction last year and everyone told me I was being dramatic. I cried for an hour after I got home. Now I have my EpiPen in my purse, my wallet, my car, and my gym bag. I even taught my cat how to use it (kidding... mostly). But seriously-this is life-changing.
Chris Davidson
The data presented is statistically significant but lacks proper citation. The 78% figure regarding delayed epinephrine administration is not sourced. Without peer-reviewed references, this reads like a fear-based marketing piece rather than medical guidance. I appreciate the intent but the credibility is compromised.
mark shortus
I WAS ALMOST DEAD. I took a single dose of ciprofloxacin and my throat closed. I thought I was dying. I couldn't breathe. I couldn't speak. I just stared at my ceiling while my wife screamed for help. They didn't give me epinephrine for 12 minutes. I had to use my neighbor's EpiPen. I'm alive because of luck. Not because the system worked. This isn't a story. This is a warning. Don't wait. Don't hope. Don't assume. ACT.
Emily P
Is there any data on the rate of false positives in penicillin allergy testing? I'm curious how many people are unnecessarily avoiding antibiotics because of a childhood rash that was never confirmed. Also, what's the long-term safety profile of repeated epinephrine use in patients who aren't truly allergic?
Jedidiah Massey
The pathophysiology of drug-induced anaphylaxis is fundamentally distinct from IgE-mediated food reactions. The complement activation cascade, particularly C3a and C5a release, plays a more dominant role in pharmacologic triggers, especially with biologics and contrast agents. This is why the kinetics are faster and the cardiovascular collapse is more profound. The current diagnostic criteria, while clinically useful, fail to account for this mechanistic divergence. We need biomarker-driven triage protocols, not symptom checklists.
Allison Pannabekcer
Thank you for writing this. I work with a lot of elderly patients who are terrified of meds because they've seen friends die from reactions. This gives me something real to share with them-not fear, but empowerment. Knowledge is the best tool we have. And yes, carry the pen. Teach someone how to use it. It's not dramatic. It's responsible.
Sarah McQuillan
Actually, I think this is a bit overblown. I'm Canadian and we don't have this level of panic over meds. People here just take their prescriptions and don't freak out. Maybe in the US it's different, but I've never seen anyone with an EpiPen just because they took a pill. This feels like American medical hysteria. We have a different culture here-calmer, more rational.