Autoimmune Disease Management: Practical Strategies for Living Well
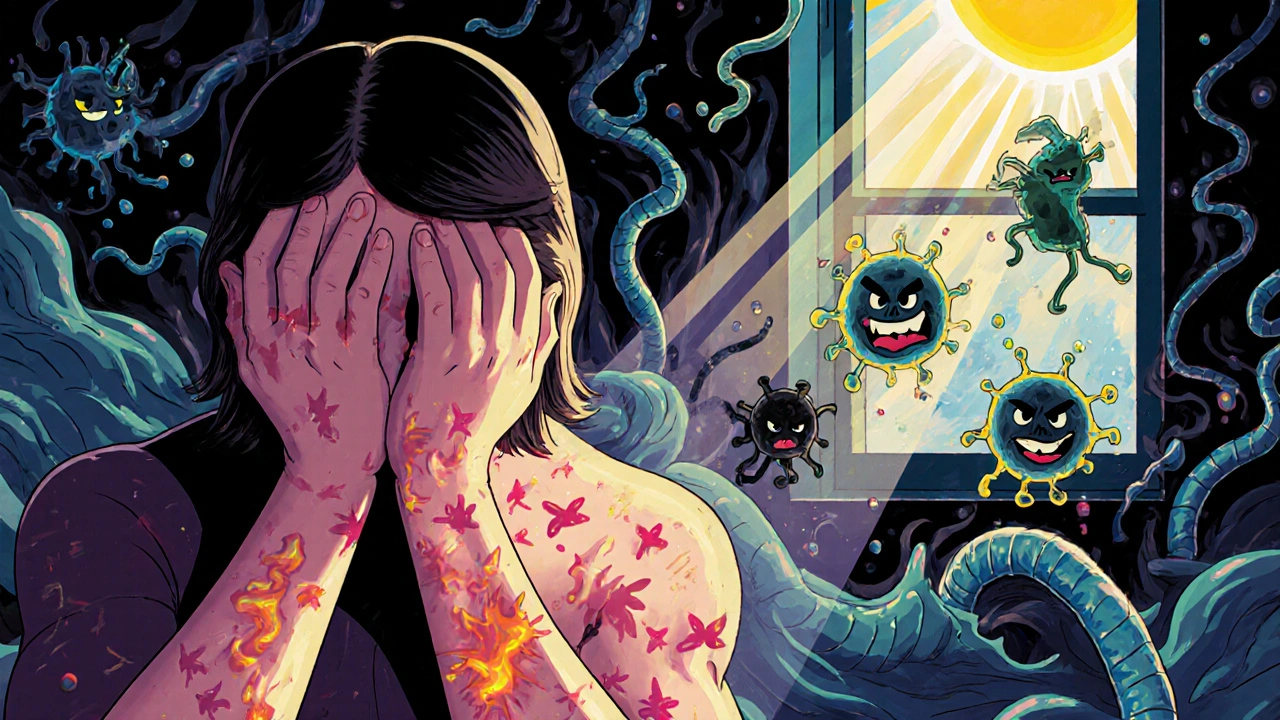
When your autoimmune disease, a condition where the immune system mistakenly attacks the body’s own tissues. Also known as autoimmune disorder, it can affect nearly any part of the body—from skin and joints to glands and organs. Autoimmune disease management isn’t about curing the problem—it’s about stopping the damage, easing symptoms, and helping you live without constant pain or fatigue. Think of it like managing a fire inside your body: you can’t always turn off the source, but you can control how hot it burns.
Common autoimmune conditions like Sjögren’s Syndrome, an autoimmune disorder that attacks moisture-producing glands, causing dry eyes and mouth and Addison’s disease, a failure of the adrenal glands that requires lifelong steroid replacement show how varied these diseases are. But they all share one thing: chronic inflammation. That’s why most management plans focus on reducing inflammation with medications like corticosteroids, immunosuppressants, or targeted biologics. But drugs alone aren’t enough. Lifestyle changes—like cutting out processed foods, getting enough sleep, and managing stress—can make a real difference. One study of people with Sjögren’s found that those who reduced sugar and refined carbs reported less fatigue and dryness within weeks.
Many people don’t realize how much immune system, the body’s defense network that, in autoimmune conditions, turns against itself is influenced by daily habits. Skipping sleep or staying stressed keeps your immune system stuck in high alert, making flare-ups worse. On the flip side, gentle movement like walking or yoga helps regulate immune signals. Even something as simple as staying hydrated supports your body’s ability to flush out toxins and keep mucous membranes moist—critical if you’re dealing with dry eyes or mouth.
Medications play a big role, but they’re not perfect. Steroids like hydrocortisone or prednisone can help control flares, but long-term use brings risks: weight gain, bone loss, high blood pressure. That’s why doctors often pair them with other drugs—like hydroxychloroquine for joint pain or low-dose naltrexone for immune balancing. And because every person’s immune system reacts differently, what works for one person might do nothing for another. That’s why tracking symptoms, keeping a food and mood journal, and working closely with your doctor matters more than any single treatment.
You’ll also find that autoimmune disease management often overlaps with other health issues. Fluid retention from medications? That’s covered in posts about diuretics and kidney disease. Hormonal imbalances? They’re linked to PCOS and thyroid conditions like hypothyroidism. Even skin rashes from autoimmune triggers can be managed with topical steroids like triamcinolone. The connections are real, and they matter.
What you’ll find below isn’t just a list of articles—it’s a practical toolkit. From how to recognize early signs of adrenal crisis to what actually helps with chronic dryness, these posts give you the facts without the fluff. No guesses. No hype. Just what works, what doesn’t, and what you need to know to take control.
Autoimmune Flares: Triggers, Prevention, and Early Intervention
Learn the real triggers behind autoimmune flares, how to prevent them with science-backed strategies, and why early intervention can cut flare duration by over six days. Practical, actionable steps for managing lupus, RA, MS, and more.