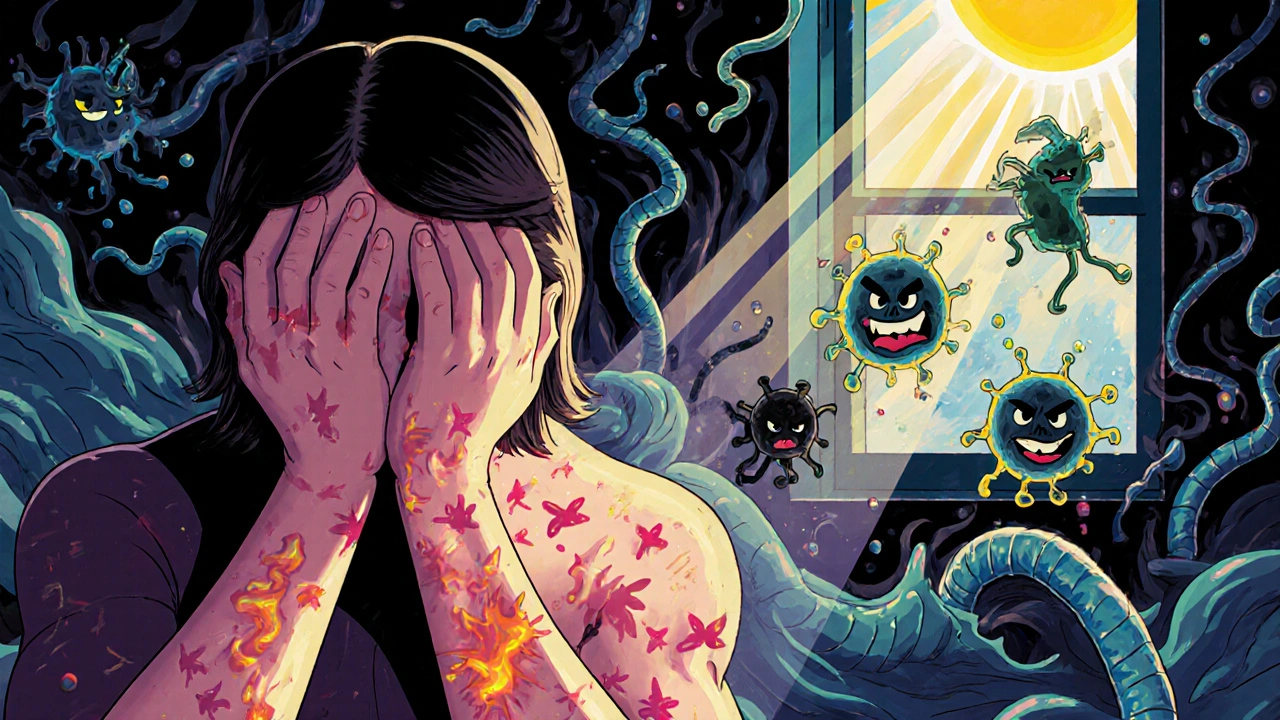
When your immune system turns on your own body, it doesn’t just cause mild discomfort-it can derail your life. Autoimmune flares are sudden, intense bursts of symptoms that can make walking, working, or even thinking feel impossible. For someone with lupus, it might mean a rash spreading across their face and joints swelling so badly they can’t hold a coffee cup. For someone with rheumatoid arthritis, it could mean being stuck in bed for days because morning stiffness lasts longer than their entire commute. These aren’t just bad days. They’re biological storms-triggered by things you might not even realize, and often preventable if you know what to look for.
What Happens During an Autoimmune Flare?
An autoimmune flare isn’t just a worsening of symptoms. It’s your immune system going rogue. Normally, your body has checkpoints that stop immune cells from attacking healthy tissue. During a flare, those checkpoints fail. T cells start mistaking your joints, skin, or kidneys for foreign invaders. B cells churn out autoantibodies that target your own organs. Cytokines-signaling molecules that should help coordinate defense-go into overdrive, flooding your body with inflammation.
This isn’t theoretical. Lab tests show clear patterns: C-reactive protein (CRP) spikes 30-50% above baseline. Erythrocyte sedimentation rate (ESR) climbs from under 20 mm/hr to 30-50 mm/hr. Autoantibody levels, like anti-dsDNA in lupus or anti-CCP in rheumatoid arthritis, can double or triple. But here’s the catch: you don’t need a lab report to know you’re flaring. Eighty-five percent of patients report crushing fatigue. Seventy-eight percent of rheumatoid arthritis patients feel new or worsening joint pain. Sixty-five percent of lupus patients describe brain fog so thick they forget words mid-sentence.
The Seven Major Triggers Behind Flares
Flares don’t come out of nowhere. Research identifies seven clear triggers-and most are within your control.
- Stress: Acute stress-like a job loss, divorce, or even a car accident-can trigger a flare within 72 hours. Cortisol, your body’s natural anti-inflammatory, gets overwhelmed. Studies show stress increases flare risk by 40-60%.
- Infections: Viruses like Epstein-Barr (the cause of mono) are notorious flare starters. About 35% of flares follow an infection. Even a common cold can tip the balance in someone with lupus or MS.
- Diet: Gluten isn’t just a problem for celiac disease-it worsens flares in 99% of those patients. High sodium intake raises relapse rates in multiple sclerosis by 30%. Sugar and processed foods fuel inflammation, making flares longer and harsher.
- UV Radiation: Sunlight isn’t just a summer concern. For people with cutaneous lupus, UV exposure causes 45% of skin flares. Even through windows, UVA rays can trigger rashes and fatigue.
- Seasonal Changes: Flares spike 37% more in spring and fall than in summer or winter. Changes in temperature, humidity, and daylight disrupt immune rhythms.
- Hormonal Shifts: Pregnancy can calm rheumatoid arthritis symptoms-but the postpartum period? That’s when 40% of women experience their worst flares. Estrogen and progesterone fluctuations directly affect immune activity.
- Medication Non-Adherence: Skipping doses of DMARDs, biologics, or steroids causes 28% of preventable flares. It’s not laziness-it’s often cost, side effects, or forgetting. But every missed pill increases risk.
Prevention Isn’t Optional-It’s Survival
You can’t eliminate flares entirely, but you can cut them in half. Prevention isn’t about miracles. It’s about consistency.
- UV Protection: Use SPF 50+ sunscreen every two hours-even on cloudy days. Wear wide-brimmed hats and UV-blocking sunglasses. One study showed this alone reduced cutaneous lupus flares by 52% over a year.
- Stress Management: Mindfulness-based stress reduction (MBSR) cut flare frequency by 35% in a 6-month trial. That’s 10 minutes of breathing, 5 days a week. No app needed. Just you, your breath, and a quiet corner.
- Dietary Changes: The Autoimmune Protocol (AIP) diet removes gluten, dairy, eggs, nightshades, and processed foods. In one study, rheumatoid arthritis patients saw a 42% drop in flare frequency. It’s not a fad-it’s an immune reset.
- Vitamin D: If your level is below 40 ng/mL, you’re at higher risk. Supplementing to reach 40-60 ng/mL lowered MS relapses by 32%. Get tested. Don’t guess.
- Medication Adherence: Use smartphone reminders. Set alarms. Link pill-taking to daily habits-like brushing your teeth. One study showed 65% better compliance with reminders-and a 28% drop in flares.

Early Intervention: The Game-Changer
Waiting until you’re bedridden is a mistake. The first 24-72 hours of a flare are critical.
The Lupus Foundation’s ‘Flare First Response’ protocol found that starting low-dose steroids within 24 hours of symptom onset reduced hospitalizations by 45% and cut flare duration by over six days. That’s not just convenience-it’s preserving your organs, your job, your independence.
What does early intervention look like?
- Recognizing the pre-flare: Many patients notice subtle signs 2-3 days before full flare: unusual tiredness, mild joint warmth, slight headache, or a weird metallic taste. Track these.
- Having a flare kit ready: Cold packs, your prescribed rescue meds, electrolyte drinks, and a list of your current meds. One survey found patients with a flare kit recovered 33% faster.
- Using telemedicine: If you feel a flare coming, don’t wait for a week-long appointment. Virtual visits let you get steroid adjustments or lab orders within hours.
Disease-Specific Flare Patterns You Need to Know
Not all flares are the same. Knowing your disease’s signature helps you spot trouble early.
- Lupus (SLE): 2.3 flares per year on average. Most involve joints (68%) and skin (35%). Kidney involvement (42%) is serious-watch for foamy urine or swollen ankles.
- Rheumatoid Arthritis: 1.8 flares yearly. The biggest red flag? Morning stiffness lasting more than 45 minutes. That’s 92% predictive of a flare.
- Multiple Sclerosis: Average relapse rate is 0.6 per year. Look for vision blurring, leg weakness, or numbness. These aren’t ‘just tired’ symptoms-they’re neurological.
- Crohn’s Disease: Flares mean abdominal pain (87%) and diarrhea (79%). Blood in stool? That’s a red flag.
- Ulcerative Colitis: Bloody diarrhea (92%) and sudden urgency (85%) are the hallmarks. No guessing here.
What Experts Are Saying Now
Dr. William Robinson at Stanford calls autoimmune flares ‘excitable dynamics of immune networks’-meaning they build slowly, then crash suddenly. The goal? Catch them before they explode.
The American College of Rheumatology now says patient-reported symptoms matter just as much as lab results. Why? Because 30% of people feel terrible-even when their CRP is normal.
And the future? It’s here. In September 2023, the FDA approved FlareGuard AI, a wearable tool that predicts flares 72 hours in advance using heart rate variability and sleep patterns. Accuracy? 76%. Meanwhile, NIH’s $15 million project is using blood tests to predict lupus flares 14 days ahead-with 82% accuracy.
But there’s a warning: overusing steroids to treat flares creates a vicious cycle. Sixty-five percent of patients on frequent steroid bursts develop osteoporosis within five years. That’s why experts now push for preventive strategies-not just reactive ones.
Real People, Real Strategies
On Reddit’s r/Autoimmune community, 72% of users say brain fog is their worst symptom. Many didn’t realize they were flaring until days later. The top tip? Track triggers in an app. Sixty-eight percent of those who tracked for three months found at least one personal pattern-like dairy causing fatigue, or stress before a meeting triggering joint pain.
One woman with lupus started using a simple Google Sheets tracker: daily entries for sleep, diet, stress level, sun exposure, and symptoms. Within weeks, she saw her flares dropped from monthly to every three months. She didn’t change her meds. She just stopped ignoring the clues.
Another man with Crohn’s kept a ‘flare kit’ in his car: prednisone, electrolyte packets, a heating pad, and a printed list of his doctors’ contact info. When he felt the first cramp, he took his med, hydrated, and called his GI. He avoided three ER visits in a year.
These aren’t outliers. They’re people who stopped waiting for a doctor to save them-and started saving themselves.
What’s the difference between a flare and regular symptoms?
Regular symptoms are your baseline-mild joint stiffness, occasional fatigue, or minor skin changes. A flare is a noticeable, measurable increase in severity or new symptoms that interfere with daily life. For example, if you usually have 15 minutes of morning stiffness and suddenly it lasts over an hour, or you develop a new rash or fever, that’s a flare.
Can I prevent flares completely?
No, you can’t prevent them 100%-autoimmune diseases are unpredictable. But you can reduce frequency and severity by 50% or more with consistent triggers management, medication adherence, and early intervention. Prevention isn’t about perfection. It’s about reducing risk.
Do I need to follow a strict diet forever?
Not necessarily. The Autoimmune Protocol (AIP) is a temporary elimination diet designed to identify your personal triggers. After 30-90 days, you slowly reintroduce foods one at a time. Many people find they can tolerate some foods again-others need to avoid them long-term. It’s personalized, not permanent.
Is stress really that big of a factor?
Yes. Stress directly impacts your immune system by disrupting cortisol and increasing inflammatory cytokines. Studies show acute stress raises flare risk by 40-60% within 72 hours. You don’t need to eliminate stress-you need to manage it. Even 10 minutes of daily breathing can make a measurable difference.
Should I take vitamin D even if I’m not deficient?
If you have an autoimmune condition, aim for serum levels above 40 ng/mL-even if your doctor says you’re ‘normal’ at 30. Research shows this level reduces MS relapses by 32% and lowers inflammation across multiple autoimmune diseases. Get tested, then supplement to reach that target.
What if my doctor doesn’t believe my flares are real?
Keep a symptom journal with dates, triggers, and severity. Include photos of rashes, notes on sleep or stress, and lab results. Use the American College of Rheumatology’s patient-reported outcome tools. If your doctor dismisses your experience, seek a second opinion from a rheumatologist or autoimmune specialist. Your symptoms are valid-even if labs are normal.
Next Steps: What to Do Today
Don’t wait for the next flare to hit. Start now.
- Download a free symptom tracker app (like CareClinic or MyTherapy) and log your symptoms daily for two weeks.
- Check your vitamin D level with a simple blood test. If it’s under 40 ng/mL, start supplementing with 2,000-5,000 IU daily.
- Build a flare kit: Keep your rescue meds, cold packs, electrolytes, and emergency contact list in one place.
- Identify your top two triggers. Maybe it’s stress or sun. Then create one small action to reduce exposure-like wearing a hat every day or setting a daily meditation reminder.
- Ask your doctor about telemedicine options for flare management. Don’t wait for a crisis to get help.
Autoimmune flares are brutal-but they’re not inevitable. You have more power than you think. Track. Prevent. Act early. Your body is fighting for you. Now it’s your turn to fight back-with knowledge, not fear.






Andrew Forthmuller
this post is wild. i didnt even know sun through windows could trigger flares. just got back from a walk and now i'm paranoid.
vanessa k
I've been tracking my symptoms for 6 months now and I can tell you, stress and sleep are the two biggest culprits for me. No magic pill, just consistency. It's exhausting but worth it.
manish kumar
Let me tell you something real. I'm from India, and here, most doctors don't even believe autoimmune diseases exist unless your labs are screaming. I had to fly to the US to get diagnosed. The AIP diet changed my life. No gluten, no dairy, no sugar. It's not easy, but when you're not crawling out of bed in pain, you learn to prioritize. I've gone from 4 flares a year to maybe one now. And yes, I track everything in a notebook. No app needed. Just pen, paper, and sheer will.
Nicole M
Anyone else get that weird metallic taste right before a flare? I thought it was just anxiety until I started journaling. Now I catch it 2 days before and prep my flare kit. Game changer.
Arpita Shukla
The FlareGuard AI thing is hype. The NIH study? Peer-reviewed? Name the journal. Also, vitamin D at 5000 IU? That's toxic long term. You're not a lab rat.
Benjamin Stöffler
We live in an age of quantified suffering-where every ache is logged, every flare is a data point, and our bodies are reduced to graphs and percentages. But what about the soul? The quiet grief of a life interrupted? The dignity of simply being tired? The algorithm doesn’t see that. It sees CRP. It sees ESR. It sees compliance rates. But it doesn’t see the woman who cried in the grocery store because she couldn’t lift her milk carton. That’s the real flare.
Mark Rutkowski
You know what’s beautiful? That we’re learning to listen to our bodies again. Not just the doctors, not just the labs-but us. The quiet whispers before the storm. The fatigue that says, ‘rest.’ The warmth in the joint that says, ‘watch out.’ This isn’t just medicine. It’s relearning how to be human in a world that wants us to push through. And that? That’s revolutionary.
Ryan Everhart
So you're telling me the solution to a complex immune disorder is... a google sheet and a hat? Cool. I'll just stop taking my $10k/month biologic and start meditating. Makes total sense.
David Barry
76% accuracy on AI flare prediction? That’s garbage. My Fitbit says I’m ‘rested’ every morning and I’m still bedridden. This whole thing is a placebo with a subscription fee.
Alyssa Lopez
AIP diet? That's just a fad for rich white ladies. In America, we got real medicine-steroids, biologics, insurance. You don't need to eat kale to survive. Just take your pills and stop whining.
Alex Ramos
I’ve been using MyTherapy for 8 months now. Best decision ever. I track meds, sleep, mood, and sun exposure. Last month, I noticed every time I ate eggs, I got joint pain 12 hours later. Cut them out. Flares dropped 70%. Also, I started using a heating pad before bed. It’s not magic, but it’s mine. You got this 💪
edgar popa
Flare kit in the car? Genius. I keep mine in my backpack now. Prednisone, electrolytes, and my dog’s leash. Because if I’m going down, she’s coming with me.
Eve Miller
You say 'preventable' flares. But the data shows 28% are due to non-adherence. That's not 'forgetting.' That's negligence. People need to take responsibility.
Chrisna Bronkhorst
This whole post reads like a pharmaceutical ad. Where's the data on long-term AIP outcomes? Who funded the FlareGuard study? And why is everyone ignoring the fact that 40% of autoimmune patients are on Medicaid? You can't afford a $500/month diet.
Amie Wilde
I just started tracking. Day 3. Already saw a pattern: bad sleep = worse flare next day. Not rocket science. But nobody told me to listen.