What Is Polycystic Ovary Syndrome (PCOS)?
Polycystic Ovary Syndrome, or PCOS, isn’t just about cysts on the ovaries. That’s a common myth. It’s a hormonal disorder that affects 5-10% of women during their reproductive years. The real problem? Your body’s hormones are out of sync. This messes with ovulation, causes unwanted hair growth or acne, and often leads to irregular or missing periods. Many women don’t realize they have PCOS until they’ve been trying to get pregnant for months-or years-and nothing’s working.
The diagnosis isn’t based on one test. Doctors look for at least two out of three signs: irregular periods (because you’re not ovulating), high levels of male hormones like testosterone (which shows up as facial hair or breakouts), and polycystic-looking ovaries on an ultrasound. But here’s the catch: you can have PCOS without cysts, and you can have cysts without PCOS. That’s why diagnosis often takes 2-3 years after symptoms start.
The Hormonal Imbalance Behind PCOS
At the heart of PCOS is a chain reaction of hormonal chaos. It starts with insulin resistance-something that affects 50-70% of women with PCOS, even if they’re not overweight. When your body can’t use insulin properly, it makes more of it to compensate. That extra insulin doesn’t just affect blood sugar-it tells your ovaries to pump out more testosterone.
Normal testosterone levels for women are around 15-25 ng/dL. In PCOS, they often jump to 20-30 ng/dL or higher. That’s why 70% of women with PCOS get hirsutism (excess hair on the face, chest, or back), 30-40% deal with stubborn acne, and 25% notice thinning hair on the scalp. At the same time, your liver produces less SHBG (sex hormone-binding globulin), which normally keeps testosterone in check. So even if total testosterone isn’t sky-high, the free, active part of it is.
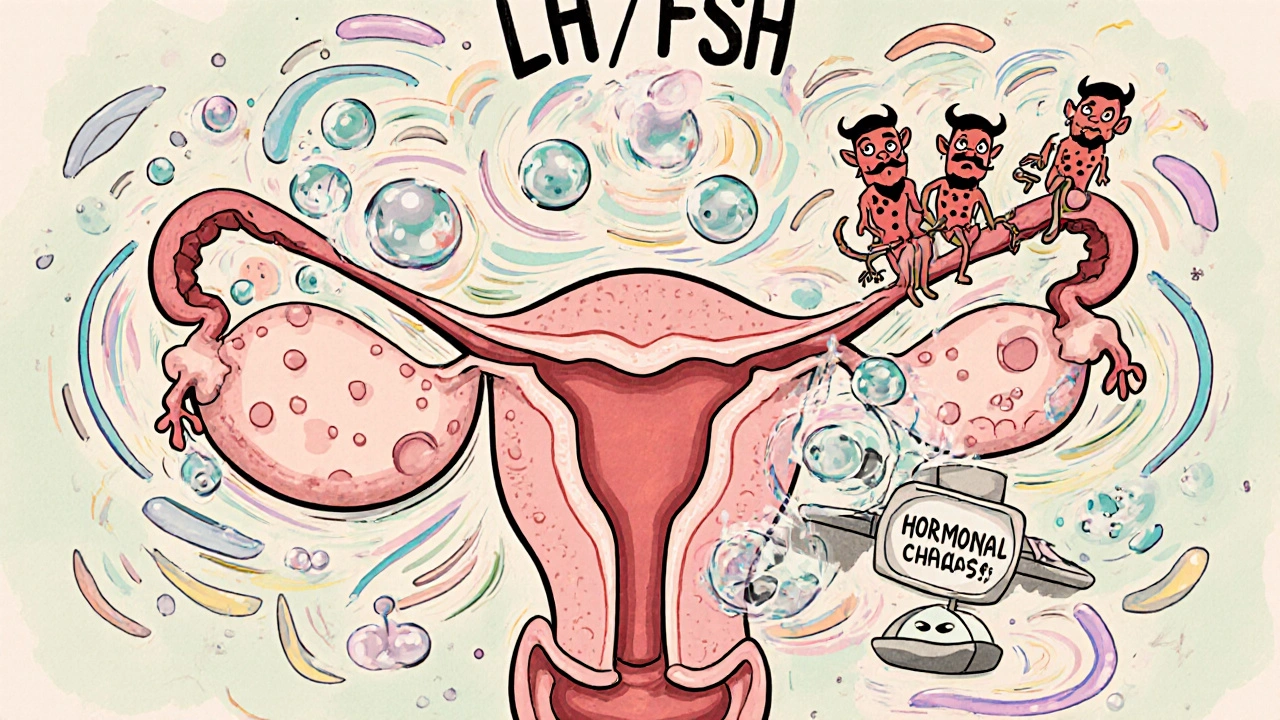
Then there’s your brain. The pituitary gland sends out LH (luteinizing hormone) and FSH (follicle-stimulating hormone) to tell your ovaries when to mature eggs. In PCOS, LH is often elevated-sometimes more than double FSH. That ratio (LH:FSH > 2:1) throws off egg development. Instead of one healthy egg maturing each month, many small follicles start growing but never release anything. That’s what shows up on ultrasound as "polycystic" ovaries.
And because you’re not ovulating, your body doesn’t make enough progesterone. Without progesterone to balance estrogen, your uterine lining keeps building up. That’s why periods are irregular, heavy, or absent. Long-term, this raises your risk of endometrial cancer by 2-6 times.
Why Fertility Is Affected-and How to Fix It
PCOS is the number one cause of anovulatory infertility. No ovulation? No egg to fertilize. But the good news? Most women with PCOS can get pregnant with the right treatment. It’s not about luck-it’s about fixing the hormonal signals.
First step? Lifestyle changes. Losing just 5-10% of body weight can restore ovulation in 30-50% of overweight women. That’s not a miracle-it’s science. Weight loss improves insulin sensitivity, lowers testosterone, and helps your brain reset the signals to your ovaries. The Diabetes Prevention Program protocol (150 minutes of walking or cycling per week plus a 500-750 calorie daily deficit) works. In studies, 44% of women who followed it started ovulating regularly within six months.
Diet matters too. A low-glycemic index diet (foods that don’t spike blood sugar) reduces insulin levels by 30% compared to standard diets. The DASH diet-originally for high blood pressure-has also been shown to improve menstrual regularity by 35% in 12 weeks. Cut out sugary drinks, refined carbs, and processed snacks. Focus on vegetables, lean proteins, whole grains, nuts, and healthy fats.

Medications That Help You Ovulate
If lifestyle changes aren’t enough, medications step in. First-line treatment is usually clomiphene citrate (Clomid). It blocks estrogen receptors in the brain, tricking your body into thinking estrogen is low. That tells your pituitary to release more FSH, which kicks off egg development. About 60-85% of women ovulate on Clomid, and 30-40% get pregnant within six cycles. Live birth rates hover around 22%.
But if Clomid doesn’t work after 3-6 cycles, letrozole (Femara) is now the preferred next step. Originally a breast cancer drug, it’s been shown to be more effective than Clomid for PCOS. In the landmark PPCOS-II trial, letrozole led to ovulation in 88% of women versus 70% on Clomid. Live birth rates? 27.5% for letrozole versus 19.1% for Clomid. Many fertility specialists now recommend letrozole as first-line, especially for women with higher BMI.
Metformin is another tool. It’s an insulin-sensitizing drug used for type 2 diabetes, but it helps PCOS too. Alone, it’s not great for ovulation-only 15-40% of women ovulate on it. But when combined with Clomid or letrozole, it boosts pregnancy rates by 30-50%, especially in women with insulin resistance or BMI over 35. Side effects? Nausea and diarrhea are common at first. Most people tolerate it better if they start low (500 mg once daily) and increase slowly.
When You Need Stronger Treatments
If pills don’t work, the next step is injectable fertility drugs called gonadotropins. These directly stimulate the ovaries with FSH and LH. They’re more powerful but come with risks. Pregnancy rates per cycle are 15-20%, but the chance of twins or triplets jumps to 20-30%. There’s also a 5-10% risk of ovarian hyperstimulation syndrome (OHSS)-a dangerous swelling of the ovaries with fluid buildup.
That’s why IVF is usually saved for cases with other infertility factors (like blocked tubes or male factor) or after multiple failed cycles. But even with IVF, PCOS patients need special care. They respond more strongly to stimulation, so doctors use lower doses of hormones (150-225 IU/day instead of 225-300 IU). Still, OHSS risk stays higher than average-10-20% versus 1-5% in non-PCOS patients. Freezing all embryos and transferring later (freeze-all strategy) helps reduce OHSS risk.
What No One Tells You About PCOS and Mental Health
PCOS doesn’t just affect your body-it hits your mind too. Depression and anxiety affect 30-50% of women with PCOS. Why? Hormonal shifts, body image struggles from weight gain or hirsutism, infertility stress, and yes-weight stigma in medical settings. A 2022 survey found 78% of women with PCOS felt judged by doctors because of their weight. 65% said they got no real diet advice, just "lose weight."
It’s not enough to treat the hormones. You need support. Talking to a therapist who understands PCOS helps. Joining a group like the PCOS Awareness Association or r/PCOS on Reddit (over 145,000 members) can make you feel less alone. Some women find mindfulness or yoga helps lower cortisol, which can worsen hormonal imbalance. Stress doesn’t cause PCOS, but it makes it worse.

What’s New in PCOS Treatment?
The field is changing fast. In 2022, the FDA approved the first digital therapy for PCOS: Femaloop PCOS, an app that gives personalized diet, exercise, and sleep plans. In trials, it improved menstrual regularity by 28% in six months.
Researchers are also testing new drugs. One combination pill-relugolix, estradiol, and norethindrone (Myfembree)-showed 89% of women had regular periods in early trials, compared to just 32% on placebo. It’s not approved for fertility yet, but it could help regulate cycles long-term.
AI is coming too. Algorithms using AMH levels, LH:FSH ratios, and ovarian volume are already predicting PCOS with 92% accuracy. In the next few years, diagnosis may be faster and more precise.
Long-Term Health Beyond Fertility
PCOS isn’t a problem you "fix" and forget. It’s a lifelong condition. Even after you have a baby, your risk of type 2 diabetes doesn’t go away. By age 40, 50% of women with PCOS will develop it. Your risk of heart disease is also doubled. That’s why annual checks for blood sugar, cholesterol, and blood pressure are non-negotiable.
Many women stop treatment once they get pregnant. Don’t. Insulin resistance doesn’t vanish after birth. Continue healthy habits. Get screened. Talk to your doctor about metformin if you’re at high risk. Your future self will thank you.
Real Stories, Real Results
One woman on BabyCenter shared: "Three failed Clomid cycles. Letrozole on the first try. Pregnant with twins at 32." Another on Reddit waited four years and saw five doctors before getting diagnosed at 28. Her periods had been irregular since age 12.
There’s no one-size-fits-all. What works for one woman might not work for another. But the pattern is clear: early diagnosis, lifestyle changes, and the right medication can turn a diagnosis of infertility into a baby in your arms.
Can you get pregnant with PCOS without medication?
Yes, some women with PCOS conceive naturally, especially if they’re at a healthy weight and have mild symptoms. Losing even 5-10% of body weight can restart ovulation without drugs. But for most women with PCOS-especially those with insulin resistance or irregular cycles-medication or fertility treatment significantly increases the chances of pregnancy.
Is metformin safe for long-term use in PCOS?
Metformin is generally safe for long-term use. It’s been used for decades to treat type 2 diabetes and is well-studied in PCOS. Common side effects like nausea and diarrhea usually improve with time or by taking it with food and slowly increasing the dose. Long-term use may help reduce diabetes risk and improve metabolic health, even if you’re not trying to get pregnant.
Why is letrozole better than Clomid for PCOS?
Letrozole works differently than Clomid. It lowers estrogen temporarily, which signals the brain to produce more FSH. Unlike Clomid, it doesn’t linger in the body and doesn’t negatively affect the uterine lining or cervical mucus. In large clinical trials, letrozole led to higher ovulation and live birth rates than Clomid in women with PCOS, making it the preferred first-line drug in many guidelines today.
Does PCOS go away after menopause?
The symptoms like irregular periods stop after menopause, but the underlying hormonal and metabolic issues don’t disappear. Women with PCOS still face higher risks of type 2 diabetes, heart disease, and metabolic syndrome after menopause. That’s why ongoing health monitoring is essential-fertility isn’t the only concern.
Can diet alone cure PCOS?
Diet alone can’t cure PCOS, but it’s the most powerful tool for managing it. A low-glycemic, anti-inflammatory diet can reverse insulin resistance, lower testosterone, and restore ovulation in many women. When combined with regular exercise, it often reduces or eliminates the need for medication. But it’s not a quick fix-it’s a lifelong commitment to health.


Christopher Robinson
Just wanted to say this post is a godsend. I’ve been Googling PCOS for months and nothing explained the insulin-testosterone link like this. I started metformin + low-glycemic diet 3 months ago and my periods are back. No more panic attacks before my OB appointments. 🙌
Angela Gutschwager
Clomid failed. Letrozole worked. 2 kids. Done.
harenee hanapi
Everyone says 'lose weight' like it's magic. I’ve lost 80 lbs. Still have PCOS. Still can't ovulate. Still get judged by nurses who say 'if you just tried harder.' Why is my body the problem but my doctor's ignorance isn't? 😔
Andy Feltus
It’s funny how medicine treats PCOS like a puzzle you solve with drugs, but ignores the fact that it’s a systemic signal failure. The body isn’t broken-it’s responding to environmental chaos. Insulin resistance? That’s not a flaw in your ovaries. It’s your cells screaming for less sugar, more sleep, less stress. We treat symptoms like criminals instead of listening to the messenger. 🤔
Nick Lesieur
So letrozole’s better than clomid? Wow. Who knew? Next you’ll tell me water’s wet. I’ve been on Clomid for 2 years and my doc just said 'maybe try letrozole?' Like, thanks for the 2024 update, Dr. Obvious. Also, I’m 35 and my insurance won’t cover letrozole for 'fertility' but will cover it for 'cancer.' What even is this system?
Timothy Reed
As someone who’s been managing PCOS for 12 years, I appreciate the depth here. The part about SHBG and free testosterone is rarely explained well. And yes-metformin + lifestyle isn’t glamorous, but it’s the foundation. I’ve seen patients skip the basics and go straight to IVF, only to burn out. This isn’t a sprint. It’s a lifestyle redesign. Keep sharing this kind of clarity.
Dion Hetemi
Let’s be real-90% of these 'success stories' are from women who were already thin or had mild PCOS. The rest of us? We’re the ones getting told 'just try harder' while our LH:FSH ratio is 5:1 and our AMH is off the charts. You talk about letrozole like it’s a cure-all. What about the 30% who don’t respond? No one talks about that. And don’t even get me started on the fact that no one tests for thyroid or prolactin before calling it PCOS. Half the time it’s something else.
Kara Binning
I’m from the Midwest and my OB literally told me 'you’re just fat, lose weight, and you’ll get pregnant.' Then I Googled PCOS and cried for an hour. I’m 31, have a 4.0 GPA, run 5Ks, and eat clean. I’m not lazy. I’m not undisciplined. I have a hormonal disorder. And now I’m on letrozole and IVF. And yes-I’m terrified. But I’m not giving up. If you’re reading this and feel alone-you’re not. We’re here.
Michael Salmon
So letrozole works better than clomid? Shocking. And metformin? Oh, the miracle diabetes drug for PCOS. But why is no one talking about the fact that the FDA approved a *digital app* as 'treatment'? We’re outsourcing hormone regulation to a smartphone? What’s next? A TikTok workout plan to reset your LH pulse? This is medical theater. Real science is being replaced by branded content. And the worst part? People think they’re empowered because they downloaded an app. Wake up.
Ellen Calnan
I was diagnosed at 22. I thought I’d never have kids. I tried everything-acupuncture, keto, chaste tree, even a naturopath who told me to 'dance with my ovaries.' Nothing worked. Then I found a functional medicine doc who tested my insulin, cortisol, and vitamin D. Turns out I was severely deficient in D and had chronic low-grade inflammation. After 6 months of supplements, sleep hygiene, and walking 45 min daily? My period returned. No meds. No IVF. I’m pregnant now at 30. It’s not about 'fixing' PCOS. It’s about listening to your body’s whispers before it screams. And yes-it’s possible. You’re not broken. You’re just out of balance. 🌱
James Ó Nuanáin
As a British physician with over two decades of clinical experience, I must commend the precision of this exposition. However, I must interject with a point of academic rigor: the assertion that letrozole is superior to clomiphene citrate in live birth rates derives primarily from the PPCOS-II trial, which-while robust-excluded women with BMI > 38. In real-world practice, particularly within the NHS, we still observe significant heterogeneity in response. Moreover, the long-term epigenetic implications of aromatase inhibition in reproductive-age women remain incompletely characterized. One must exercise caution before institutionalizing protocols without longitudinal data. The pursuit of fertility must not eclipse the pursuit of health.