When your child needs a medicine that doesn’t come in a store-bought bottle, you might be told about compounded medications. These are custom-made by pharmacists to fit your child’s exact needs-like a liquid form for a toddler who can’t swallow pills, or a flavor that doesn’t taste like medicine. But here’s the hard truth: compounded medications aren’t tested or approved by the FDA. That means no one guarantees they’re safe, strong enough, or even made cleanly. For kids, especially babies and toddlers, a tiny mistake can mean a trip to the ER-or worse.
Why Compounded Medications Are Used for Kids
Most kids don’t need compounded drugs. FDA-approved medicines exist for common conditions: ear infections, asthma, seizures, thyroid problems. But sometimes, those don’t work. Maybe your child is allergic to dyes or preservatives in commercial pills. Maybe they’re too small for the lowest available dose. Or maybe they gag at the taste of liquid antibiotics and won’t take it at all. That’s where compounding comes in. Pharmacists can make:- Sugar-free liquids for diabetic kids
- Alcohol- and dye-free formulas for sensitive children
- Flavored syrups with strawberry or bubblegum taste to hide bitter drugs
- Ultra-low doses of strong medicines like morphine or fentanyl for newborns in NICUs
- Preservative-free injectables for premature babies
The Hidden Dangers of Compounded Medications
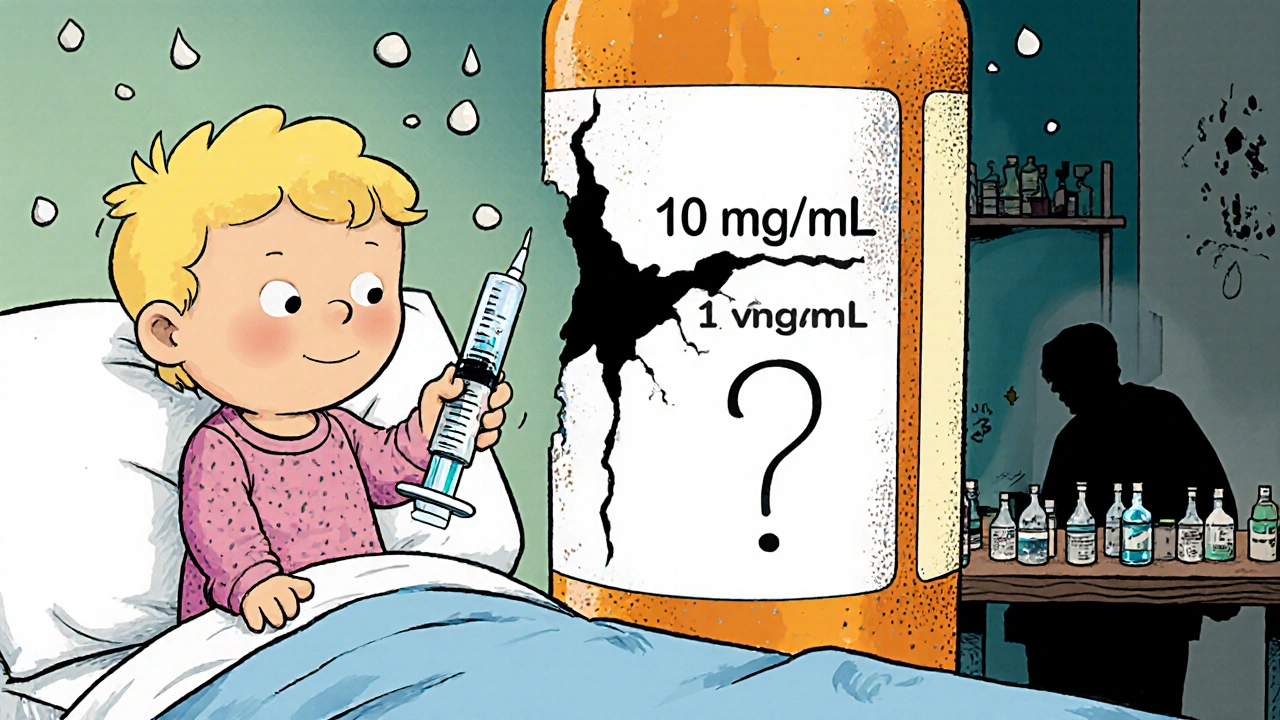
You might think, “It’s made by a pharmacist, so it’s safe.” That’s not true. Unlike factory-made drugs, compounded medications aren’t checked for purity, strength, or consistency. The FDA doesn’t approve them. That’s not a loophole-it’s a gap in protection. In 2022, the Institute for Safe Medication Practices found that 14% to 31% of pediatric medication errors involve compounded drugs. Most of these are dosing mistakes. A child weighing 15 pounds needs a fraction of the dose a 70-pound child needs. If the concentration is wrong-say, 10 mg/mL instead of 1 mg/mL-that’s a tenfold overdose. One drop too much can cause seizures, breathing trouble, or organ damage. There are real cases. In 2006, a two-year-old girl named Emily Jerry died after a compounded chemotherapy dose was mixed wrong. The pharmacy used the wrong syringe and gave her 10 times the intended dose. Her death sparked a national movement. Yet, ten years later, similar errors still happen. A parent on Reddit shared that their 8-year-old ended up in the ER after taking compounded levothyroxine. The pharmacy delivered a batch that was 40% weaker than prescribed. The child developed hypothyroid symptoms: fatigue, weight gain, cold intolerance. Another family reported vomiting and diarrhea after a compounded version of semaglutide-a drug meant for adults with obesity or diabetes-was given to their child. The FDA logged over 900 adverse events linked to compounded semaglutide and tirzepatide by the end of 2024, including 17 deaths. Children were disproportionately affected. Contamination is another risk. In 2012, a fungal meningitis outbreak killed 64 people and sickened nearly 800 after contaminated steroid injections were compounded in a single pharmacy. The source? Dirty equipment and poor hygiene. That outbreak led to new laws-but many small pharmacies still cut corners.When Should You Avoid Compounded Medications?
The FDA is clear: compounded drugs should only be used when no FDA-approved alternative exists. That’s the rule. But many pharmacies now make compounded versions of popular drugs like semaglutide or tirzepatide-even when those drugs are available as approved, branded products. For children, this is especially dangerous. Why? Because:- Children’s bodies process drugs differently than adults
- Small changes in dose have big effects
- There’s no safety net-no large-scale testing, no post-market monitoring
How to Spot a Safe Compounding Pharmacy
Not all compounding pharmacies are the same. Some follow strict rules. Others operate like DIY labs. Here’s how to tell the difference:- Look for PCAB or NABP accreditation. The Pharmacy Compounding Accreditation Board (PCAB) and the National Association of Boards of Pharmacy (NABP) set high standards. Only about 1,400 of the 7,200 compounding pharmacies in the U.S. have this seal. Ask for proof.
- Ask if they use gravimetric analysis. This is a high-tech method that weighs ingredients down to the milligram instead of using volume measurements. It cuts dosing errors by 75%. But only 7.7% of U.S. hospitals use it, mostly because it costs $25,000-$50,000 per station. If the pharmacy says they don’t have it, ask why-and whether they do double-checks.
- Check their state license. All compounding pharmacies must be licensed by their state pharmacy board. You can verify this online through your state’s board of pharmacy website.
- Ask about training. Pharmacists who compound for children should have at least 40 hours of specialized training in pediatric dosing. Ask if their technicians are certified in sterile compounding under USP Chapter <797>.
What Every Parent Must Do Before Giving a Compounded Medicine
Even the best pharmacy can make a mistake. You are your child’s last line of defense. Here’s your checklist:- Get the exact concentration. Always ask: “What’s the strength? Is it 5 mg/mL? 10 mg/mL?” Many errors happen because parents think they’re giving 2 mL when the bottle says 1 mg/mL, but the label was misprinted as 10 mg/mL. Write it down.
- Double-check with two people. Ask the pharmacist to explain the dose. Then ask your child’s doctor to confirm it. Don’t rely on memory. Use the written instructions.
- Use the right measuring tool. Never use a kitchen spoon. Use the syringe or dosing cup the pharmacy gives you. If they didn’t give one, ask for it. A teaspoon holds 5 mL. A tablespoon holds 15 mL. But syringes are precise. Get one with clear markings.
- Store it correctly. Some compounded liquids need refrigeration. Others must be used within 14 days. Ask: “How long does this last? What happens if it’s left out?”
- Watch for side effects. If your child gets vomiting, diarrhea, drowsiness, rash, or unusual crying after starting the medication, stop it and call the doctor immediately. Don’t wait.
What to Do If Something Goes Wrong
If you suspect a compounding error-your child got the wrong dose, or reacted badly-act fast.- Stop the medication. Don’t wait to see if it gets better.
- Call your pediatrician or go to the ER. Bring the medicine bottle and the prescription with you.
- Report it. File a report with the FDA’s MedWatch program. You can do it online or by phone. This helps track dangerous patterns.
- Save the bottle. Even if it’s empty, keep it. The pharmacy may need to investigate.
- Ask for a new batch. If the pharmacy made a mistake, they should provide a new, verified dose at no cost.
The Bigger Picture: Why This Problem Keeps Growing
The market for compounded medications hit $11.3 billion in 2024-and it’s growing fast. But pediatric use? Just 8.2% of that total. Still, the risks are highest for kids. Why? Because their bodies are small, fragile, and sensitive. A mistake that’s minor for an adult can be deadly for a child. Some pharmacies are taking advantage of drug shortages to make and sell compounded versions of popular drugs-even after the shortage ends. The FDA says this is illegal, but enforcement is slow. Meanwhile, parents are left to guess whether the medicine they’re giving their child is safe. The solution isn’t to ban compounding. It’s to demand better. More pharmacies need to invest in gravimetric machines. More pharmacists need specialized training. More states need to pass laws like “Emily’s Law,” which requires gravimetric verification for pediatric sterile compounds. So far, 28 states have introduced such bills. Until then, parents must be vigilant. You can’t control the pharmacy. But you can control what you ask, what you check, and what you refuse to accept.Are compounded medications safe for children?
Compounded medications can be safe when used correctly and when made by an accredited pharmacy using strict standards. But they are not FDA-approved, so there’s no guarantee of quality, strength, or safety. For children, especially infants and toddlers, even small errors in dosage can lead to serious harm. They should only be used when no FDA-approved alternative exists.
How do I know if my child’s compounded medication is made safely?
Look for a pharmacy with PCAB or NABP accreditation. Ask if they use gravimetric analysis (weighing ingredients instead of measuring by volume). Check that their staff is trained in USP Chapter <797> for sterile compounding. Always ask for the exact concentration and verify it with your doctor and pharmacist.
Can I use a regular syringe from home to give the medicine?
No. Never use a kitchen spoon or household syringe. Always use the dosing tool provided by the pharmacy. Household tools are inaccurate and can lead to overdoses or underdoses. If no tool was provided, call the pharmacy and ask for one. A proper oral syringe has clear markings and is designed for precise dosing.
What should I do if my child has a bad reaction to a compounded medication?
Stop giving the medication immediately. Contact your child’s doctor or go to the emergency room. Bring the medication bottle and prescription with you. Report the reaction to the FDA’s MedWatch program. Save the bottle-even if it’s empty-so the pharmacy can investigate.
Is it okay to use compounded versions of drugs like semaglutide for my child?
No. Semaglutide and tirzepatide are FDA-approved for adults with obesity or type 2 diabetes. They are not approved for children, and compounded versions have been linked to over 900 adverse events-including 17 deaths-as of December 2024. These drugs were never meant for pediatric use. Giving them to children, even in compounded form, is dangerous and not medically supported.
Why don’t more pharmacies use gravimetric analysis if it’s so much safer?
Gravimetric analysis requires expensive equipment ($25,000-$50,000 per station) and extensive staff training. Many small pharmacies, especially in rural areas, can’t afford it. Labor costs and time delays also make it harder to adopt. But studies show it reduces pediatric dosing errors by 75%. Without widespread adoption, preventable errors will continue to happen.







Miriam Lohrum
It's wild how we trust pharmacists like they're magicians, but the system's built on trust, not proof. I get that compounding saves lives when there's no alternative, but why is it so easy for a mom to get a vial of something with no batch number, no testing, and no way to trace it back? We regulate toothpaste better than we regulate life-saving pediatric meds.
It's not about fear-it's about accountability. If a car part fails, we recall the whole model. If a pill kills a kid, we get a press release and a footnote in a federal report. Where's the justice in that?
archana das
I live in India and we see this a lot-parents ask for flavored syrups because kids refuse pills. But here, even the big pharmacies don’t have standards. I once saw a child given a compounded antibiotic that looked like pink paint. No label, no concentration, just a cup and a prayer.
We need global rules. Not just for the US. Kids everywhere deserve safe medicine, not luck.
Emma Dovener
My son had a severe allergy to dyes in commercial amoxicillin. We were lucky-we found a PCAB-accredited pharmacy that used gravimetric analysis. But it took three months of calling 17 pharmacies before we found one. Most didn’t even know what PCAB stood for.
Don’t assume your pharmacist knows. Ask. And if they look confused, walk out.
Sue Haskett
Okay, I’m going to say this again, and again, and again: NEVER, NEVER, NEVER use a kitchen spoon. NEVER. I’ve seen it. I’ve seen the ER reports. I’ve seen the parents crying because they thought ‘a teaspoon’ meant the one from their silverware drawer. It’s not a suggestion. It’s a life-or-death rule. Use the syringe. Always. And if they don’t give you one-demand it. Your child is not a lab rat.
Jauregui Goudy
This post is a wake-up call. I used to think compounding was some fancy pharmacy magic. Now I know it’s a gamble. And we’re betting our kids’ lives on it.
That story about Emily Jerry? I cried. And then I called my pediatrician and asked if any of our meds were compounded. Turns out, one was-because the ‘standard’ version had corn syrup in it. We switched. Immediately.
If you’re not asking these questions, you’re not parenting-you’re hoping.
Tom Shepherd
so i just found out my kid’s thyroid med is compounded and i had no idea. the label just said ‘levothyroxine 0.05mg/ml’ and i assumed it was the same as the brand. turns out it was 40% weaker. he was tired all the time, gaining weight, cold all the time. we only caught it because his teacher said he was zoning out in class. i’m so mad. why didn’t anyone tell me?
Rhiana Grob
There’s a balance here. Compounded medications are not inherently dangerous-they are under-regulated. The issue isn’t the practice, it’s the lack of oversight. We need to invest in pharmacy infrastructure, not vilify pharmacists. Many of them work in tiny clinics with no funding, trying to help children who otherwise have no options.
The solution is not fear-it’s funding. Training. Standards. And holding the big players accountable when they compound drugs like semaglutide for kids just because they can profit from it.
Frances Melendez
Of course your kid got sick. You didn’t even check if the pharmacy was accredited. You just took the doctor’s word and trusted the ‘nice pharmacist’ with the smile. You think your child is special? Every parent thinks that. But the system doesn’t care about your feelings. It cares about standards. And you didn’t demand them.
You’re lucky they didn’t die. Next time, do your homework-or don’t complain when the ER lights flash.
Jonah Thunderbolt
Look. I’m a biochemist. I’ve worked in compounding labs. The truth? 90% of these pharmacies are glorified kitchen operations. They use graduated cylinders. They don’t calibrate. They don’t validate. And they charge $300 for a vial of ‘custom’ morphine that could be 1 mg/mL or 10 mg/mL. It’s a carnival.
And don’t get me started on semaglutide for kids. That’s not medicine. That’s pharmaceutical snake oil. The FDA should shut these places down. Not regulate them. Shut them down. 💀
Rebecca Price
Let’s be real: the fact that we’re even having this conversation is a failure. We have the technology to make pediatric meds safe. Gravimetric analysis. Batch tracking. Standardized concentrations. But we don’t fund it. We don’t require it. We don’t enforce it.
And then we blame parents for not knowing the difference between a syringe and a teaspoon.
It’s not your fault. It’s the system’s. And until we treat pediatric compounding like the high-risk, high-stakes field it is-children will keep getting hurt. And we’ll keep saying, ‘We didn’t know.’
Well. Now you know.
shawn monroe
Gravimetric analysis = gold standard. Volume-based = gambling. Period. The fact that only 7.7% of hospitals use it is a national disgrace. We spend billions on MRI machines but won’t spend $50K to prevent a kid from getting 10x their dose? That’s not negligence-that’s systemic malice.
And don’t even get me started on the compounding pharmacies that market ‘adult weight-loss drugs’ to parents of 5-year-olds. That’s not compounding. That’s predatory. FDA needs to come in with a SWAT team and shut these down. 🔥
Miriam Lohrum
Rebecca Price said it best: it’s not the parents’ fault. But here’s the kicker-when you report a bad batch to MedWatch, 90% of the time, nothing happens. The pharmacy isn’t fined. The pharmacist isn’t suspended. The vial just disappears from the shelves, and another one gets made next week.
We need a public registry. Every compounded pediatric med should have a barcode. You scan it, you see the batch, the date, the analyst, the verification method. No excuses. No shadows.
Until then? We’re all just guessing.