You’ve heard chatter that a heart and blood pressure drug might also lift mood. Here’s the straight answer: eplerenone isn’t an antidepressant or anti-anxiety medicine, and there’s no solid clinical trial proof that taking it will treat anxiety or depression in the general population. That said, in people with high aldosterone states-like primary aldosteronism-treating the hormone problem (with surgery or mineralocorticoid receptor blockers such as eplerenone) can improve mood, energy, and quality of life. If you’re on eplerenone already and wondering about mental health effects, or you’re dealing with anxiety or depression and looking at every option, this guide gives you a realistic read.
- TL;DR: Key takeaways
- Eplerenone is not an approved or proven treatment for anxiety or depression.
- Some patients with aldosterone excess report fewer mood symptoms after treatment, but data for eplerenone specifically are limited.
- If you have heart failure or hypertension and also have depression/anxiety, stick with evidence-based mental health care; don’t add eplerenone for mood alone.
- Watch for drug interactions and potassium issues if you take eplerenone with psychiatric meds.
- Talk to your clinician before changing anything-there are safer, better-studied options for mood disorders.
What we know so far: eplerenone, stress hormones, and mood
Eplerenone blocks the mineralocorticoid receptor (MR). That’s the receptor for aldosterone, the hormone that tells your kidneys to hold onto salt and water-and raise blood pressure. MR also sits in the brain areas tied to stress and memory, like the hippocampus and amygdala. So it’s reasonable to ask whether blocking MR changes anxiety or mood. The short answer: maybe in special situations, but this isn’t a go-to mood treatment.
First, what is eplerenone actually for? It’s FDA-approved for heart failure with reduced ejection fraction (including after a heart attack) and for hypertension. Big trials like EPHESUS (2003) and EMPHASIS-HF (2011) showed survival and hospitalization benefits in heart failure. None of those trials were designed to test anxiety or depression outcomes.
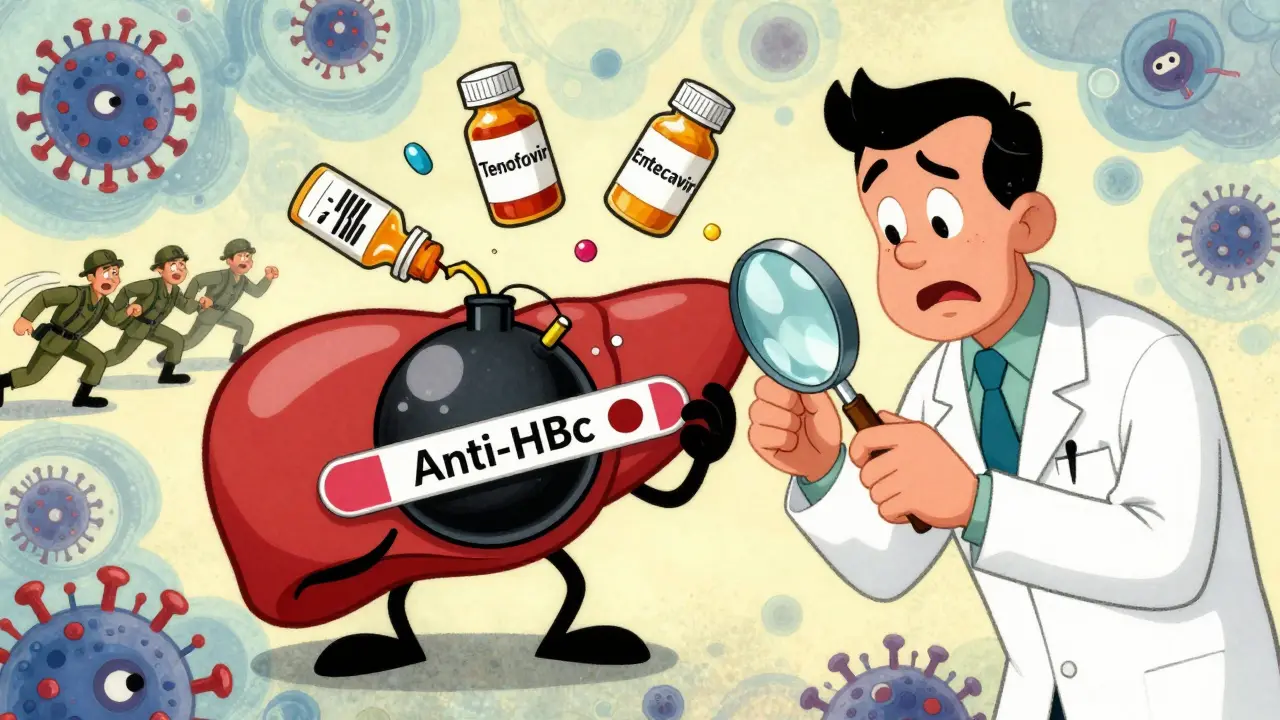
Now, the mental health angle. People with primary aldosteronism-a condition where the body makes too much aldosterone-often feel “wired and tired”: poor sleep, headaches, irritability, and yes, higher rates of depression and anxiety compared with patients who have essential hypertension. The Endocrine Society’s guideline on primary aldosteronism (2016; updated 2023) notes this burden and recommends treating the aldosterone excess with surgery (adrenalectomy for unilateral disease) or MR blockers (spironolactone or eplerenone) for bilateral disease. Observational studies and patient-reported outcomes show that after successful treatment, quality of life and mood frequently improve. In plain terms: fix the hormone problem, and some mental symptoms calm down.
Where does eplerenone specifically fit? A handful of small or observational studies suggest MR blockade may ease some stress-related symptoms, but most of the mixed evidence comes from spironolactone or from adrenal surgery cohorts. Eplerenone is more selective than spironolactone (so fewer sex-hormone side effects), but it’s also less potent milligram-for-milligram. Data directly linking eplerenone to improvements in clinical depression or generalized anxiety disorder are thin as of 2024.
What about basic science? Animal studies show that MR overactivity can heighten stress responses, and MR blockade can tweak anxiety-like behavior. Human lab studies around stress, memory, and MR/cortisol interactions hint at nuanced effects. But that’s a long walk from proving a medication treats major depressive disorder in real life.
Practical translation: if your anxiety or depression stems from everyday causes, trauma, or a primary mood disorder, eplerenone isn’t the fix. If you have proven aldosterone excess-and your doctor prescribes eplerenone to treat blood pressure and potassium issues-your mood may improve as your body’s stress-salt system settles down. That’s a bonus, not the main goal.
| Question | What the evidence says (as of 2024) | Type of evidence |
|---|---|---|
| Does eplerenone treat major depression? | No proven benefit; not an approved indication | No randomized trials for this outcome |
| Does eplerenone treat generalized anxiety? | No direct evidence of clinical benefit | No randomized trials for this outcome |
| In primary aldosteronism, do mood symptoms improve with treatment? | Often yes-quality of life and mood scores improve after adrenalectomy or MR blockade | Observational studies, patient-reported outcomes, guideline consensus |
| Is MR relevant to stress response? | Yes-MR is expressed in hippocampus/amygdala and modulates stress circuits | Basic science, small human lab studies |
Safety first: interactions, side effects, and who might benefit
If you’re taking or considering eplerenone, the safety checklist matters more than the hype. This drug raises potassium and can drop blood pressure-great when that’s the goal, risky if unmanaged.
Key safety points (people on heart meds and psych meds, read this twice):
- Potassium: Eplerenone is potassium-sparing. Hyperkalemia risk goes up with ACE inhibitors, ARBs, ARNIs, potassium supplements, potassium salt substitutes, and kidney disease. Your team will monitor potassium and kidney function.
- Blood pressure: It can lower BP. Add dizziness, dehydration, alcohol, or other BP meds and you may feel lightheaded.
- CYP3A4 metabolism: Strong CYP3A4 inhibitors can spike eplerenone levels. Contraindicated examples include ketoconazole, itraconazole, ritonavir, clarithromycin, and nefazodone (an antidepressant that’s rarely used today but still out there in charts). Moderate inhibitors (like verapamil and erythromycin) may require dose adjustments.
- Lithium: Potassium-sparing diuretics can raise lithium levels. Data on eplerenone are limited, but play it safe: check lithium more often when starting or changing the dose.
- Other psych meds: SSRIs/SNRIs generally don’t interact pharmacokinetically with eplerenone, but SSRIs can cause hyponatremia, and eplerenone can shift electrolytes the other way. Report confusion, severe fatigue, or muscle weakness fast.
- St. John’s wort: It can lower eplerenone levels (CYP3A4 induction), possibly blunting blood pressure control. Tell your clinician about supplements.
Who might notice mood changes with eplerenone?
- People with confirmed primary aldosteronism starting MR blockade: as blood pressure stabilizes and potassium normalizes, some report better sleep, less irritability, and more steady energy.
- Heart failure patients with depression: depression is common in heart failure. Treating heart failure well improves daily function, which can indirectly help mood. That’s not the same as eplerenone acting as an antidepressant.
Who should not chase eplerenone for mood?
- Anyone with regular depression or anxiety without evidence of aldosterone excess. Use proven treatments first-line.
- People with advanced kidney disease, very high baseline potassium, or on strong CYP3A4 inhibitors-unless a specialist is closely managing it.
Side effects to watch for:
- High potassium: muscle weakness, palpitations, or in severe cases, dangerous heart rhythms. This is why labs matter.
- Dizziness or low blood pressure: especially when standing up quickly.
- Kidney function changes: usually mild but important to monitor.
- Breast tenderness or hormonal effects are much less common with eplerenone than with spironolactone.
Bottom line on safety: if you’re taking eplerenone for your heart or blood pressure, you can safely combine it with most antidepressants or therapy plans, with a few interaction watch-outs. But don’t add eplerenone hoping it will treat mood on its own.
How to decide and what to do next (simple steps that work)
If your question is “Should I try eplerenone for anxiety or depression?” use this quick decision path.
- Start with the why. Are you considering eplerenone for blood pressure/heart failure, or purely for mood? If it’s purely for mood, skip to step 6-there are better options.
- Rule out aldosterone excess if you have resistant hypertension or unexplained low potassium. If your blood pressure is hard to control on three meds (including a diuretic), or you’ve had low potassium without a clear cause, talk to your clinician about screening for primary aldosteronism (plasma aldosterone/renin testing). Treating aldosterone excess can improve life on many fronts, sometimes including mood.
- Already on eplerenone? Track what changes. For 4-8 weeks, note weekly: mood (1-10), anxiety (1-10), sleep hours/quality, energy, and any side effects. Bring this to follow-ups. If your heart failure symptoms improve, expect indirect mood gains from better stamina.
- Check interactions before you start. Make a one-page med list with every prescription, over-the-counter pill, and supplement. Highlight: ACEi/ARB/ARNI, potassium, lithium, and any CYP3A4 inhibitors or inducers. Share it with your prescriber and pharmacist.
- Plan labs. Ask when to check potassium and kidney function (often at baseline, 1-2 weeks after starting or changing dose, then periodically). Put reminders on your calendar.
- For mood treatment, pick evidence-based options. First-line for depression and most anxiety disorders: cognitive behavioral therapy (CBT), SSRIs/SNRIs, or both-per APA and NICE guidelines. Lifestyle levers with real impact: regular exercise (150 minutes/week), structured sleep, and reducing alcohol. If first-line fails, step up to second-line meds or augmentation based on guideline algorithms.
What should you ask your clinician?
- “Given my blood pressure and labs, should we screen for primary aldosteronism?”
- “If I start eplerenone, how often will we check potassium and kidney function?”
- “Do any of my meds or supplements interact with eplerenone?”
- “What’s our plan for my depression/anxiety that uses treatments with the best evidence?”
- “How will we measure progress-PHQ‑9, GAD‑7, or both-and when will we adjust?”
A quick case example: A 42-year-old with tough-to-control hypertension (three meds) and low potassium feels anxious, sleeps 5 hours a night, and has frequent headaches. Screening shows high aldosterone with suppressed renin. After targeted treatment (adrenalectomy for unilateral disease or MR blocker for bilateral disease), blood pressure normalizes and potassium levels stabilize. Within a few months, she reports fewer panic-like episodes and better sleep. Notice what changed: the root cause (aldosterone excess) was treated. That’s different from using eplerenone to treat primary anxiety or depression without an endocrine driver.
Pro tips that save headaches:
- Don’t use potassium-based salt substitutes while on eplerenone unless your clinician says it’s okay.
- Stay consistent with lab appointments; most scary side effects are predictable and preventable with labs.
- If you take lithium, schedule a level 5-7 days after any eplerenone dose change.
- If dizziness hits, check your blood pressure sitting and standing. Hydrate, and tell your clinician if it keeps happening.
- For mental health, track PHQ‑9 (depression) and GAD‑7 (anxiety) scores monthly. Small, steady improvements matter.
FAQs, quick checks, and next steps
Is eplerenone an antidepressant? No. It’s a mineralocorticoid receptor blocker used for heart failure and hypertension. There’s no approval or strong trial evidence showing it treats depression.
Can eplerenone help anxiety? Not directly. Some people with aldosterone excess feel calmer after treatment, but that’s likely from fixing the hormone imbalance, not from a universal anti-anxiety effect. If you searched eplerenone anxiety, that’s the nuance you were looking for.
Does it cross into the brain? Eplerenone is more selective for MR than spironolactone and may have limited central nervous system penetration. Even so, MR signaling affects stress pathways. The clinical impact on mood remains unclear.
Can I swap spironolactone for eplerenone for mood reasons? If you’re switching because of spironolactone side effects (breast tenderness, menstrual changes), eplerenone is a reasonable alternative for blood pressure/heart indications. Don’t expect the switch to change mood on its own.
Any special concerns with antidepressants? Watch interactions, not synergy. Nefazodone is a no-go (strong CYP3A4 inhibitor). Be mindful of lithium levels. Most SSRIs/SNRIs are fine with normal lab monitoring.
What about pregnancy or breastfeeding? Eplerenone safety data in pregnancy are limited; decisions should be individualized with cardiology and obstetrics. For mood in pregnancy, psychotherapy and certain SSRIs have more data. Don’t start or stop anything without talking to your care team.
How do major guidelines view this? The Endocrine Society recommends treating primary aldosteronism because it improves cardiovascular and quality-of-life outcomes. The American Psychiatric Association and NICE recommend psychotherapy and antidepressants as first-line for depression and for most anxiety disorders. No mainstream mental health guideline recommends eplerenone to treat mood disorders.
What results should I expect if I’m starting eplerenone for heart failure? You may notice less fluid retention, better exercise tolerance, and fewer hospitalizations over time. Any mood lift would likely be indirect-feeling better because your heart is working better.
Red flags to call your clinician about quickly:
- New or worsening suicidal thoughts
- Severe muscle weakness, palpitations, or fainting (possible high potassium)
- Confusion, seizures, severe nausea (possible electrolyte imbalance)
- Persistent dizziness with standing
Cheat-sheet: safe use with psych meds
- SSRIs/SNRIs: typically compatible; monitor electrolytes and blood pressure.
- Bupropion: generally okay; watch blood pressure if you’re sensitive.
- Mirtazapine: compatible; appetite/weight changes can affect BP management.
- TCAs: monitor for blood pressure effects and anticholinergic burden.
- Antipsychotics: many are CYP3A4 substrates, but not strong inhibitors; check the specific drug.
- Nefazodone: avoid with eplerenone (strong CYP3A4 inhibitor).
- Lithium: monitor levels after starting or adjusting dose.
Next steps by persona
- If you’re a patient with hard-to-control blood pressure and mood symptoms: ask about aldosterone screening. If positive, treat the root cause; mood may follow.
- If you’re already on eplerenone: keep your lab schedule, track mood weekly for 2 months, and keep your therapy/med plan steady unless you and your clinician decide otherwise.
- If you’re seeking help for anxiety or depression without heart/BP issues: book a visit to discuss first-line treatments with proven benefits (CBT, SSRIs/SNRIs). Don’t chase off-label MR blockers.
- If you’re a clinician: consider PHQ‑9/GAD‑7 at baseline and follow-up for patients starting MRAs, especially those with suspected primary aldosteronism. Make interaction checks routine-especially CYP3A4 issues and potassium risk.
Where the research is headed: Scientists are still mapping how MR and glucocorticoid receptors dance together under stress. Maybe one day we’ll see targeted MR strategies for certain stress-related conditions. As of 2024, the clinical playbook for mood disorders is unchanged: stick to therapies and meds with strong evidence, and treat underlying endocrine problems when they exist.
Quick reference-when to think about MR and mood:
- Resistant hypertension + low potassium + anxiety/irritability → screen for aldosterone excess.
- Starting eplerenone for heart reasons → track energy and sleep; mood gains may be indirect.
- No heart/BP issues, just anxiety/depression → see your primary care or psychiatry team for guideline-based care.
Helpful numbers to remember:
- Lab timing: often baseline, 1-2 weeks after starting/adjusting, then every 1-3 months early on.
- Exercise target: 150 minutes/week of moderate activity for mood and heart health.
- Sleep: aim for 7-9 hours; set a consistent bedtime to stabilize stress hormones.
Final note: If you landed here searching for a hidden fix, I get it. But the safe, reliable path wins: treat the right problem with the right tools. Eplerenone can be a hero for the heart. For anxiety or depression, you’ve got better, proven options-and those are the ones that change lives.





Mer Amour
Eplerenone isn't some miracle mood drug. People keep chasing biological shortcuts like it's a magic pill, but if your anxiety is real, you need therapy, not a heart med that happens to have a side effect of feeling less wired. This isn't biohacking-it's basic medicine. Stop conflating symptom relief with treatment.
And yes, I've seen it in clinic: patients with primary aldosteronism do feel better after treatment, but that's because their body stopped flooding with aldosterone. It's not eplerenone lifting their mood-it's fixing the endocrine chaos. Don't turn a niche physiological correction into a general mental health solution.
There are 12 FDA-approved antidepressants. Twelve. Pick one. Or do CBT. Or both. Don't waste time on off-label stabs at hormones unless your labs scream aldosterone excess.
I'm tired of Reddit turning every obscure drug into a 'secret cure' for anxiety. It's dangerous. And lazy.
Cosmas Opurum
USA doctors pushing eplerenone for mood? Typical. First they give you antidepressants that make you numb, then they say 'maybe it's your potassium'.
They don't want you to know the real cause: corporate pharma wants you dependent on pills. Aldosterone? Too cheap to patent. But eplerenone? That's a billion-dollar drug. They'll sell you the bottle and call it 'mental health' while your real problem-stress, pollution, processed food-is ignored.
I've seen this in Nigeria too. Western doctors overcomplicate everything. Fix your diet. Sleep. Move. Stop chasing pills that 'might' help. The system is rigged.
And don't get me started on CYP3A4 inhibitors. That's just a fancy way to scare you into more lab tests. You don't need 12 labs a year to feel better.
Real medicine is simple. They just don't want you to know that.
peter richardson
I'm on eplerenone for heart failure and I swear my anxiety dropped after 3 weeks
Not because it's an antidepressant
But because I stopped feeling like I was gonna pass out every time I stood up
My BP used to crash hard
Now I can walk to the fridge without needing a nap
That's not magic
That's just not being sick anymore
Don't turn that into a mood drug claim
It's just better function
And yeah potassium labs matter
I almost died once from ignoring them
Don't be that guy
Uttam Patel
So let me get this straight
You're telling me the same drug that gives men boobs (spironolactone) might also make you feel less like crying?
Wow
Science is wild
Next you'll say Prozac is just a fancy diuretic
Look I get it
You're desperate
But please don't turn a heart med into your new therapist
Also if you're taking St. John's wort with this
Go ahead and jump off a bridge
At least you'll die happy
Kirk Elifson
They don't want you to know this
But eplerenone is part of the Great Mental Health Cover-Up
Big Pharma doesn't profit from treating aldosterone excess
They profit from selling SSRIs to millions of people who just need to fix their salt balance
Why do you think depression rates exploded after 2005?
Because we stopped screening for primary aldosteronism
It's all connected
They call it 'essential hypertension'
But it's not essential
It's suppressed
And your anxiety? It's your adrenal glands screaming for help
Not your brain
Ask your doctor for plasma aldosterone testing
Or keep swallowing pills and wondering why you still feel empty
Wake up
The system is lying to you
Nolan Kiser
Let me cut through the noise. Eplerenone is not an antidepressant. Period.
But if you have resistant hypertension + low potassium + chronic fatigue + irritability - you absolutely need to get screened for primary aldosteronism. It’s underdiagnosed by 80% in the US. And yes, when you fix that, people report better sleep, less panic, more energy. It’s not the drug ‘treating depression’ - it’s removing a physiological burden that was making everything worse.
Think of it like this: if you have a broken leg and you’re depressed because you can’t walk, fixing the leg helps your mood. That doesn’t mean crutches are antidepressants.
Also - if you’re on lithium, check your levels 5–7 days after starting eplerenone. That’s not optional. That’s life-saving.
And if you’re just anxious and not hypertensive? Please, for your own sake, talk to a therapist or try an SSRI. Don’t gamble with potassium levels chasing a myth.
This isn’t about drugs. It’s about matching the right tool to the right problem.
Yaseen Muhammad
Thank you for this comprehensive, evidence-based breakdown. Too often, online discussions reduce complex medical topics to binary claims: 'this drug cures depression' or 'it's useless.' The truth lies in nuance - and this post nails it.
Patients with primary aldosteronism often experience psychiatric symptoms secondary to hormonal dysregulation. Correcting the underlying pathophysiology can yield profound improvements in quality of life - including mood - but this is not equivalent to treating major depressive disorder or generalized anxiety disorder with eplerenone.
It's critical to distinguish between indirect benefit and direct therapeutic effect. The former is real and valuable; the latter is unsupported.
Also, I appreciate the emphasis on potassium monitoring and CYP3A4 interactions. These are easily overlooked, especially when patients are managing multiple medications. A simple med list and scheduled labs can prevent serious harm.
For anyone reading this: if you're struggling with mood, please seek care from a mental health professional. Evidence-based treatments exist. They work. And they're safer than chasing off-label drug effects.
Medical humility and scientific rigor - these are the real heroes here.