When a patient is switched from a brand-name NTI drug to a generic version, the stakes are higher than with most medications. These aren’t ordinary drugs. A tiny change in blood levels-just a few percentage points-can mean the difference between effective treatment and serious harm. For drugs like warfarin, phenytoin, digoxin, or levothyroxine, even small shifts in how the body absorbs the medicine can lead to clots, seizures, heart rhythm problems, or thyroid failure. Yet, many patients are never told why the switch is happening, or what to watch for afterward.
Why NTI Drugs Are Different
Narrow Therapeutic Index (NTI) drugs have a razor-thin margin between the dose that works and the dose that’s dangerous. The FDA defines them as medications where small changes in blood concentration can cause treatment failure or life-threatening side effects. For example, warfarin must keep a patient’s INR between 2 and 3. Go slightly above? Risk of bleeding. Go slightly below? Risk of stroke. digoxin works best between 0.5 and 0.9 ng/mL. Go over that? Toxicity. Go under? No effect.
Generic versions of these drugs must meet stricter standards than regular generics. While most generics only need to show 80% to 125% similarity in absorption compared to the brand, NTI generics must hit 90% to 111.11%. For drugs like levothyroxine, the bar is even higher-AUC must fall between 95% and 105%. These numbers aren’t arbitrary. They come from years of clinical data and FDA analysis. But patients don’t know this. And too often, neither do providers.
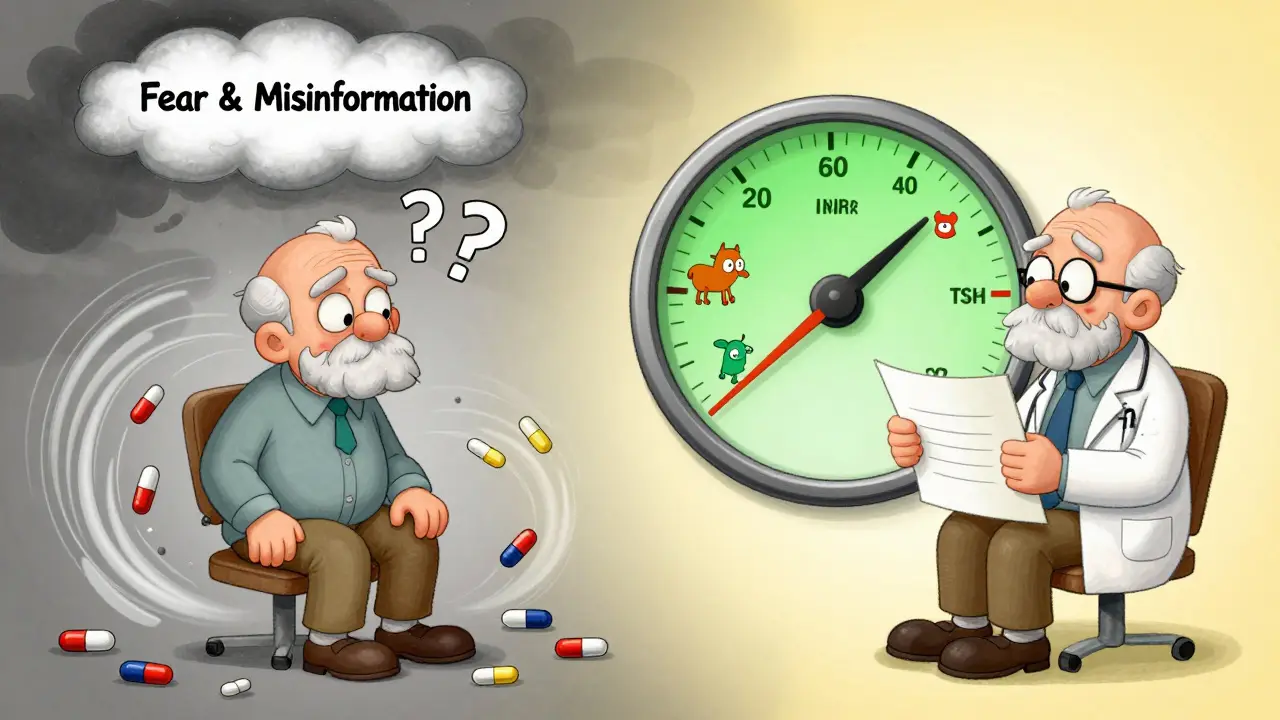
What Patients Really Fear
When you tell a patient, "We’re switching you to a generic," they hear: "I’m getting a cheaper version." That’s not what you mean. But that’s what they believe. A 2017 survey found that 60% of pharmacists still hesitate to substitute generic NTI drugs-even though 94% believed they were safe. That hesitation trickles down. Patients pick up on it. They worry the generic won’t work. They’ve heard stories. Maybe they know someone who had a seizure after switching antiepileptics. Or they read online that generics aren’t "the same."
The truth? The FDA has approved these generics. They’ve been tested. But trust isn’t built with data sheets. It’s built with conversation.
What You Need to Say
Don’t say: "This is just a generic." Say: "This is the exact same medicine, tested to work the same way in your body. I prescribe it for my own family." That’s not just a script. It’s a shift in tone. You’re not explaining a policy. You’re acting as a trusted advisor. Patients remember who speaks with certainty and care.
Here’s what to cover:
- "It’s the same medicine." Emphasize that the active ingredient is identical. No filler, no placebo. The same molecule.
- "It’s been tested more than most brand-name drugs." Explain the 90-111% bioequivalence range. Compare it to the looser 80-125% for regular generics. Show them this isn’t a compromise-it’s a tighter standard.
- "We’ll check your levels." For warfarin, monitor INR in 3-5 days. For phenytoin or valproic acid, check serum levels in 7-10 days. For levothyroxine, TSH in 6-8 weeks. Don’t just say "we’ll monitor." Say when, how, and why.
- "If you feel different, call us." Tell them exactly what symptoms to watch for: unusual bruising, dizziness, confusion, heart palpitations, tremors, or fatigue. Don’t assume they’ll know what’s normal.
Use the FDA’s own language: "This generic version has been tested to deliver the same amount of medicine into your bloodstream as the brand version. We’ll check your blood levels in one week to make sure everything is working correctly."

State Laws and What You Must Do
As of 2024, 27 states have specific rules about NTI drug substitution. Fourteen require written patient consent before switching. Others require pharmacists to notify the prescriber. In Australia, while there’s no federal NTI-specific law, state pharmacy boards follow guidelines aligned with the Therapeutic Goods Administration (TGA), which recommends full disclosure and monitoring. You must know your local rules. If your state requires consent, don’t skip it. Document it. Have the patient sign. Keep a copy. It’s not bureaucracy-it’s protection.
And here’s something many miss: It’s not just about the first switch. If a patient is switched again-say, from Generic A to Generic B-that’s another change. Each time, they need to be counseled again. You can’t assume they remember what you said last month.
Who’s at Higher Risk?
Some patients are more vulnerable. Elderly patients. Those with kidney or liver problems. People on five or more medications. Patients with poor health literacy. These groups need extra attention. A 2023 study found that patients over 65 were 40% more likely to have a medication-related problem after switching NTI generics. Why? Slower metabolism. More drug interactions. Harder to notice subtle changes.
For these patients, use visual aids. Show them a chart of the therapeutic window. Point to where their level should be. Use simple analogies: "Think of it like a car’s speedometer. We need to keep it at 60-not 55, not 65. This generic keeps it right where it should be."
What the Data Shows
Here’s what really matters: patients who get proper education have 28% fewer problems after switching. Those who get visual aids have 42% higher adherence. That’s not small. That’s life-changing.
Between 2019 and 2023, the FDA recorded 1,247 adverse event reports linked to NTI drug switches. But only 17% were proven to be caused by the switch itself. Most were due to missed monitoring, not the drug. That’s the real problem-not the generic. It’s the lack of follow-up.
What You Should Do Next
- Check your state’s NTI substitution laws. Know if consent is required.
- Use the FDA’s 2024 NTI Communication Toolkit. It has ready-made scripts in 12 languages.
- Train your staff. Pharmacists who use teach-back methods (ask patients to repeat the info in their own words) see 35% better outcomes.
- Document everything: "Patient counseled on therapeutic equivalence of [drug], advised to monitor [test] within [timeframe], provided educational materials."
- Follow up. Don’t wait for them to call. Send a text or make a quick call three days after the switch. "How are you feeling? Any new symptoms?"
Why This Matters More Than You Think
NTI drugs make up only 3.2% of all generic approvals-but they cause 11.7% of patient questions about generics. That’s because people are scared. And when they’re scared, they stop taking their medicine. Or they switch back to the brand, even if it costs $200 a month. That’s not just expensive. It’s dangerous.
Good communication isn’t optional. It’s clinical care. When you take the time to explain, you don’t just prevent problems. You build trust. You give patients control. And you help them stay safe.
Are generic NTI drugs really as safe as brand-name drugs?
Yes. The FDA requires generic NTI drugs to meet stricter bioequivalence standards than regular generics. For most NTI drugs, the amount of medicine absorbed into the bloodstream must fall within 90% to 111.11% of the brand version-much tighter than the 80%-125% range for other drugs. Drugs like warfarin, phenytoin, and levothyroxine have been tested in thousands of patients. Studies show they work just as well. The real risk isn’t the generic-it’s not monitoring after the switch.
Why do some pharmacists refuse to substitute generic NTI drugs?
Some pharmacists, especially those with decades of experience, were trained during a time when generic NTI drugs were less common and less rigorously tested. A 2017 survey found pharmacists with over 20 years of experience were 37% less likely to substitute than newer pharmacists. Also, state laws in 14 states require patient consent before substitution, which can make pharmacists hesitant to proceed without it. But FDA data since 2019 confirms these generics are safe. Education and updated guidelines are helping close this gap.
How soon after switching should I check blood levels?
It depends on the drug. For warfarin, check INR within 3-5 days. For phenytoin or valproic acid, check serum levels in 7-10 days. For levothyroxine, check TSH in 6-8 weeks. For digoxin, check levels in 5-7 days. Always follow the specific guidance for the drug being switched. The goal is to catch any unexpected change before it causes harm.
Can I switch back to the brand if I’m worried?
Yes, but only after talking to your provider. Switching back and forth between brands and generics can cause instability in blood levels, especially with NTI drugs. If you feel different after switching, don’t stop the medicine or switch on your own. Call your doctor. They may want to check your levels first. Often, symptoms aren’t caused by the drug change-they’re caused by stress, illness, or other medications. Your provider can help sort it out.
What if I’m on multiple medications?
Combining NTI drugs with other medications increases your risk. For example, if you’re on warfarin and also take an antibiotic or an antifungal, your INR can swing dangerously. The same goes for phenytoin and many common drugs. Always tell your pharmacist and doctor about every medication you take-including over-the-counter pills, supplements, and herbal products. They need to check for interactions before any switch.
Final Thought
Switching to a generic NTI drug isn’t a cost-cutting move. It’s a clinical decision. And like any clinical decision, it needs care, clarity, and follow-up. The science is solid. The data is clear. What’s missing is the conversation. When you take five minutes to explain-not just inform-you don’t just prevent problems. You save lives.





Suzette Smith
I switched my mom to generic levothyroxine last year and she’s never felt better. No more brain fog, no more crashes after lunch. I was skeptical too, but her TSH is perfect now. Sometimes the cheapest option is the best one. 🤷♀️
Autumn Frankart
They don’t want you to know this, but the FDA and Big Pharma have a secret deal. Generics are filled with fillers from China that cause silent organ damage. My cousin’s thyroid shut down after a switch. They covered it up. Look up FDA Form 3500 - it’s redacted.
andres az
Bioequivalence metrics are statistically noisy. The 90–111% range is a legal fiction. Real-world pharmacokinetic variance exceeds that threshold in 18% of elderly patients. You’re not ‘saving money’ - you’re gambling with CYP450 metabolism. Don’t confuse regulatory approval with clinical safety.
Stephon Devereux
This is why medicine needs heart, not just data. I had a patient once who cried because she thought her new generic was ‘fake.’ I pulled up the FDA’s own bioequivalence charts, showed her the molecule diagrams, and said, ‘This is the same medicine your grandpa took - just cheaper.’ She hugged me. That’s care. That’s healing.
steve sunio
u r all dumb. generic = bad. u dont know what is in it. my uncle died. u think u r smart? u r just part of the system. lol. no monitoring? nope. just take it and shut up. #pharmaracistscam
Sonja Stoces
I switched to generic warfarin and my INR went from 2.3 to 4.1 in 72 hours. I almost bled out. Now I pay $180/month for brand. My doctor said ‘it happens.’ I said ‘then why don’t you warn people?’ 😔
Rob Turner
In the UK, we don’t even have this debate. The NHS uses generics for everything, including NTIs, and monitors closely. It works. We’ve got a national database tracking outcomes. Maybe the problem isn’t the drug - it’s the lack of coordinated care. We need systems, not speeches.
Luke Trouten
There’s a difference between ‘equivalent’ and ‘identical.’ The molecule is the same, yes - but the excipients, the coating, the dissolution rate - those aren’t. For some patients, especially with GI issues, that tiny difference matters. We need personalized monitoring, not blanket policies.
Rachidi Toupé GAGNON
Geniuses don’t need brand names. They need results. 🚀 My dad’s on generic phenytoin - no seizures, no hospital trips. He says it’s like driving a Honda instead of a BMW - same road, same destination, way better gas mileage. 💪
Neha Motiwala
I’ve been on levothyroxine for 12 years... I switched to generic... I felt like I was drowning... my hair fell out... I gained 20 pounds... I begged to go back... they said ‘it’s the same’... it’s NOT the same... I’m not a lab rat... I’m a human being... 😭
athmaja biju
In India, we use generics for everything. We don’t have luxury of brand drugs. But we have doctors who monitor. We have labs that test. We have patients who know their numbers. It’s not about the label. It’s about the system. America is broken.
Craig Staszak
I’ve been prescribing NTI generics for 15 years. I’ve never had a patient with a true adverse event tied to the generic itself. The real issue? Patients stop taking it because they’re scared. Or they switch back and forth. That’s what kills. Not the pill. The panic.
alex clo
The FDA’s 90–111% standard is rigorous. But it’s not foolproof. We need real-time therapeutic drug monitoring for high-risk patients. Not just TSH or INR - we need pharmacogenomic screening. That’s the future.
Alyssa Williams
I’m a nurse. I’ve seen it all. One time I had a 78-year-old man who thought his generic digoxin was ‘poison.’ I sat with him for 20 minutes. Showed him the bottle. Said ‘this is the same as the one you’ve been on for 10 years.’ He cried. Said ‘I just needed to hear someone say it.’
Ernie Simsek
Bro. I switched to generic warfarin. My INR went from 2.5 to 1.8. I didn’t tell anyone. I just started eating more kale. Now I’m at 2.2. Problem solved. 🍃😂 #lifehacks #genericwin