Medication Weight Impact Calculator
Medication Weight Impact Calculator
Select a medication to see weight impact information.
Many people start a new medication expecting relief from pain, anxiety, or high blood pressure - not a sudden change in their weight. But it happens more often than you think. About one in four prescription drugs can cause noticeable weight gain or loss, sometimes without you realizing why. This isn’t just about looking different in the mirror. It’s about your metabolism, your energy, your risk for heart disease, and even how well your treatment works.
Why Do Medications Change Your Weight?
It’s not magic. It’s biology. Drugs interact with your body in specific ways, and weight changes are often a side effect of those interactions. There are five main ways this happens.Some medications make you hungrier. Antidepressants like mirtazapine and older antipsychotics like olanzapine affect serotonin receptors in your brain, especially the 5-HT2C receptor. When this receptor is blocked, your appetite doesn’t shut off like it should. Studies show up to 78% of long-term users report increased hunger - even when they’re eating the same amount as before.
Others store fat more easily. Diabetes drugs called thiazolidinediones (like pioglitazone) turn on PPAR-γ receptors, which basically tell your body to make more fat cells. In some cases, fat cell production jumps by 40-60%. That’s not just a few extra pounds - it’s a change in how your body stores energy.
Some drugs slow your metabolism. Beta-blockers like propranolol, often used for high blood pressure or heart conditions, reduce your resting metabolic rate by 8-10%. That means even when you’re sitting still, you’re burning fewer calories than you used to. Over months, that adds up.
Fluid retention is another common culprit. Steroids like prednisone cause your body to hold onto water. It’s not fat - it’s temporary swelling. But it can add 2-5 kg in just the first month. People often think they’ve gained weight when they’re really just bloated.
And then there’s movement. Antipsychotics and some sedatives make you tired. A 2022 Mayo Clinic study found patients on these drugs took 1,200 to 2,500 fewer steps per day. That’s like losing a 20-minute walk every single day. Over time, that lack of activity becomes a major factor in weight gain.
Which Medications Cause Weight Gain?
Not all drugs affect weight the same way. Some are notorious, others are neutral - and a few actually help you lose weight.Antidepressants show the biggest split. Paroxetine and mirtazapine often lead to 2.5-5 kg of weight gain in six months. But bupropion? It’s one of the few antidepressants linked to weight loss - about 1.5-2.5 kg over a year. That’s why doctors often choose bupropion for patients already struggling with weight.
Antipsychotics are another big category. Olanzapine causes 4.5-6 kg of weight gain in just 10 weeks. That’s why it’s avoided in patients with obesity or diabetes. But aripiprazole? It causes almost no change - just 0.2-0.8 kg. The difference isn’t random. It’s tied to how each drug binds to brain receptors.
Diabetes medications are the most dramatic. Insulin and sulfonylureas make you gain 2-4 kg in the first year. That’s because they push glucose into your cells - and if you’re not burning it off, your body stores it as fat. But newer drugs like semaglutide and liraglutide (GLP-1 analogues) do the opposite. In clinical trials, people lost 6-10 kg over six months - and kept it off. These drugs work by reducing appetite and slowing digestion.
Even birth control pills and corticosteroids can cause weight gain. It’s not always the same for everyone - genetics, diet, activity level, and how long you take the drug all play a role. But if you’ve gained more than 2.5 kg in the first few months of starting a new medication, it’s worth asking if the drug is the cause.
Which Medications Help You Lose Weight?
Not all weight changes are bad. Some drugs are now being prescribed specifically to help people lose weight - even if they were originally meant for something else.GLP-1 receptor agonists like semaglutide (Wegovy, Ozempic) and liraglutide (Saxenda) are the most powerful. In the STEP trials, patients lost 15% of their body weight on average over 68 weeks. That’s not a fluke. These drugs mimic a natural hormone that tells your brain you’re full. They reduce cravings, slow stomach emptying, and lower blood sugar - all at once.
Bupropion, as mentioned earlier, is another. It’s often paired with naltrexone (in Contrave) to boost weight loss effects. This combo reduces appetite and blocks the reward centers in the brain that drive overeating.
Even some blood pressure meds like ACE inhibitors and ARBs are linked to small but consistent weight loss - around 1-2 kg over a year. That’s because they reduce fluid retention and improve insulin sensitivity.
The key difference? These drugs don’t just suppress appetite - they change how your body regulates energy. That’s why their effects are stronger and more lasting than old-school diet pills.

What Should You Do If You’re Gaining Weight on Medication?
The first thing to remember: don’t stop taking your medication without talking to your doctor. Stopping suddenly can be dangerous.Instead, start with these four steps:
- Track your weight weekly. Use the same scale, at the same time of day. A gain of more than 2.5 kg in the first 3-6 months is a red flag.
- Review your meds with your doctor. Ask: “Is this drug known to cause weight gain? Are there alternatives with less metabolic impact?”
- Use a risk tool. Doctors can use the Liverpool University Drug Interaction Group’s weight gain prediction algorithm. It’s 87% accurate and helps compare risks across options.
- Start lifestyle changes early. Even small changes help. Add 10 minutes of walking daily. Cut sugary drinks. Focus on protein and fiber. These don’t need to be drastic - just consistent.
Many patients don’t realize their doctor didn’t warn them. A 2024 survey found only 38% of people were told about possible weight changes before starting a new drug. That’s a gap. If your doctor didn’t mention it, ask. It’s your right to know.
How Doctors Are Changing How They Prescribe
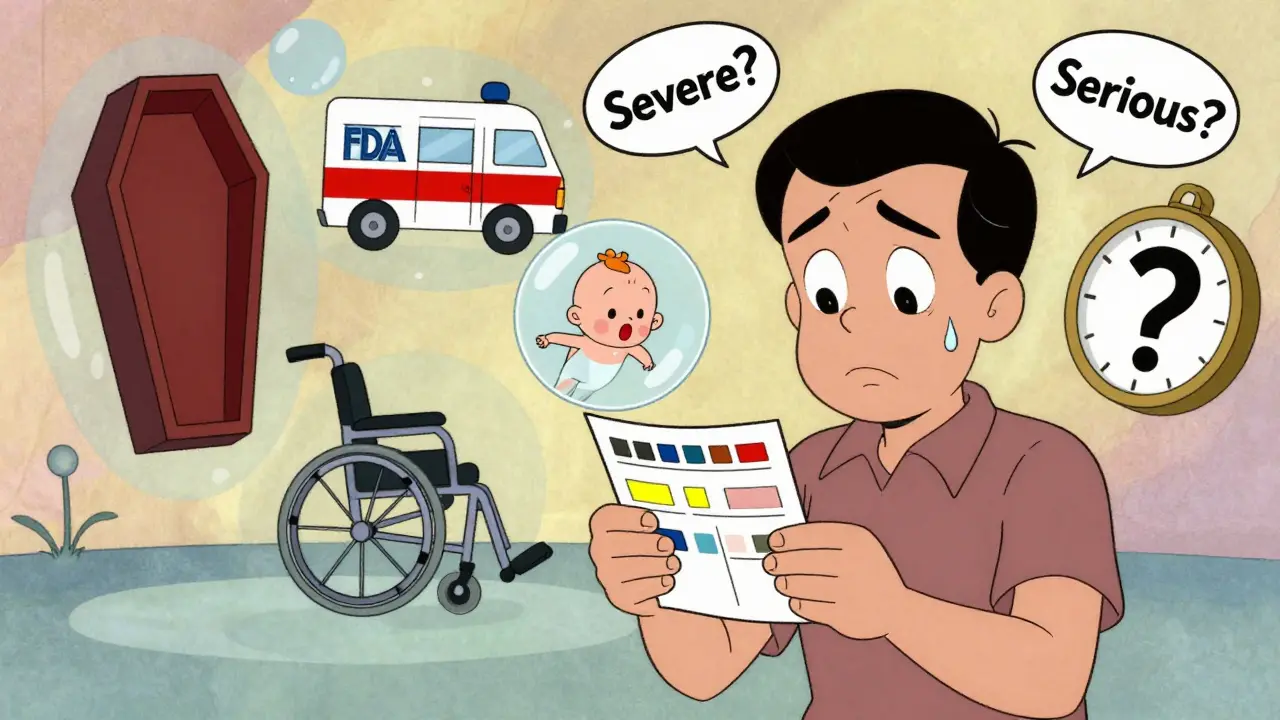
The medical community is waking up. Five years ago, weight gain was often ignored. Now, it’s part of the decision-making process.Since 2021, the FDA requires all new psychiatric drugs to include detailed weight change data in their labels. That means you’ll see numbers like “average weight gain: 3.2 kg at 12 weeks” - not just a vague note in the side effects section.
Some hospitals now offer metabolic risk assessments before prescribing. At academic centers, pharmacists and dietitians work together to choose medications that won’t sabotage your health goals. And with the NIH’s $150 million Medication-Weight Initiative launching in 2024, we’re seeing real progress toward developing weight-neutral versions of common drugs.
Pharmacogenomics is also changing the game. Testing for gene variants like HTR2C can now predict if you’re likely to gain weight on certain antipsychotics - with 79% accuracy. That means your doctor might soon order a simple blood test before prescribing, not just guess based on your history.
Employers are catching on too. Fifty-eight of the top 100 U.S. companies now include weight impact in their drug formulary decisions. Why? Because medication-induced weight gain increases healthcare costs - and absenteeism - by up to 18%.

Real People, Real Stories
Behind the data are real lives.One Reddit user, ‘AnxietyWarrior87’, gained 18 pounds on sertraline. She ate the same, exercised the same - but the scale kept climbing. After six months, she switched to bupropion. She lost the weight and says her anxiety is better managed.
Another, ‘DiabetesJourney’, switched from insulin to semaglutide. She lost 22 pounds, her blood sugar stabilized, and she no longer needs to inject insulin twice a day.
But it’s not always easy. A 2022 WHO survey found 61% of patients who gained weight on meds reported lower self-esteem. Some stopped taking their drugs because they felt ashamed. That’s why counseling matters - not just about food, but about identity and mental health.
Dr. Caroline Apovian from Boston University says: “Medication-induced weight gain is preventable.” And she’s right. With the right choices - and early action - most people can avoid gaining 3-5 kg in the first year.
What You Can Do Today
You don’t need to wait for your next appointment. Start now:- Write down every medication you take - including supplements.
- Check your weight from when you started each one. Did it change?
- Look up your drugs on Drugs.com or Medscape. Read the side effects section - look for “weight gain” or “weight loss.”
- Ask your doctor: “Is this drug likely to affect my weight? What are the alternatives?”
- Don’t be afraid to say: “I’m concerned about weight gain. Can we pick something else?”
Weight changes from meds aren’t your fault. They’re a biological side effect - not a failure of willpower. But you have power in how you respond. With the right information and support, you can stay healthy - without sacrificing your treatment or your body.
Can antidepressants cause weight gain?
Yes, some antidepressants can cause weight gain, but not all. Medications like mirtazapine and paroxetine are more likely to lead to 2.5-5 kg of weight gain within six months due to increased appetite. Others, like bupropion, are linked to weight loss. The difference comes down to how each drug affects brain chemicals like serotonin and norepinephrine. If weight gain is a concern, talk to your doctor about switching to a more weight-neutral option.
Do all antipsychotics make you gain weight?
No. While drugs like olanzapine and clozapine are strongly linked to weight gain - often 4-6 kg in the first few months - others like aripiprazole and lurasidone have minimal impact. The difference is in how they bind to receptors in the brain. Newer antipsychotics are designed to avoid those receptors, reducing side effects. Your doctor can choose a medication that treats your symptoms without triggering significant weight gain.
Can I lose weight while taking insulin?
It’s harder, but possible. Insulin helps your body store glucose as fat, which can lead to weight gain. But combining insulin with GLP-1 receptor agonists (like semaglutide) can reduce this effect. Studies show this combo leads to 4.2 kg less weight gain than insulin alone. Lifestyle changes - like eating fewer refined carbs and increasing physical activity - also help. Never stop insulin without medical supervision, but do ask about adding weight-friendly strategies.
How quickly do weight changes happen after starting a new drug?
It varies. For drugs like prednisone, fluid retention can cause a 2-5 kg increase in just the first month. For antidepressants or antipsychotics, weight gain usually starts within 4-8 weeks and continues slowly over months. GLP-1 drugs like semaglutide show weight loss within 2-4 weeks. Monitoring your weight weekly during the first 3-6 months is the best way to catch changes early.
Should I avoid medications that cause weight gain?
Not necessarily. Sometimes the mental or physical health benefits outweigh the risk of weight gain - especially if you’re managing a serious condition like depression, bipolar disorder, or diabetes. The key is awareness and planning. Work with your doctor to choose the safest option, monitor your weight closely, and add lifestyle support. Avoiding a needed medication can be riskier than managing the side effect.
Are there tests to predict if I’ll gain weight on a certain drug?
Yes - and they’re becoming more common. Genetic tests like Genomind’s Mental Health Map can analyze your HTR2C gene variant to predict your risk of weight gain from antipsychotics and some antidepressants. Accuracy is around 79%. Some academic medical centers now offer this testing before prescribing. While not yet standard everywhere, it’s a growing tool for personalized care.
What’s the best way to manage weight gain from medication?
Start with three things: regular weight tracking (weekly), dietary adjustments (focus on protein, fiber, and whole foods), and movement (even 10-15 minutes of walking daily). Combine this with a conversation with your doctor about alternatives. If needed, ask about adding a weight-loss medication like semaglutide or bupropion. Many clinics now offer metabolic support as part of routine care. You don’t have to manage this alone.



Laurie Sala
Okay, but like… why does EVERYTHING make me gain weight?? I’m on sertraline, beta-blockers, and a tiny bit of prednisone for allergies-and I’ve gained 12 lbs in 5 months even though I’m eating salad like it’s my job?? I didn’t sign up for this body. I just wanted to stop crying in the shower.
Lisa Detanna
As someone who switched from olanzapine to aripiprazole, I can say this: the difference isn’t just in the numbers-it’s in how you feel in your own skin. I went from hiding in baggy clothes to wearing jeans again. It’s not just about weight-it’s about dignity. Doctors need to stop treating this like a side note.
Demi-Louise Brown
It is imperative to acknowledge that medication-induced weight changes are a physiological phenomenon and not a reflection of personal discipline. A structured approach involving regular monitoring, collaborative physician consultation, and evidence-based lifestyle interventions remains the most effective strategy for mitigation.
Matthew Mahar
ok so i just started abilify and i swear i feel like a balloon that got left in the sun?? like i wake up and my face is puffy and my jeans dont fit and i havent even changed my diet?? this is wild. also i think i might have gained 5lbs in 2 weeks??
John Mackaill
For years, I was told to just 'eat less and move more' when I gained weight on my blood pressure meds. No one mentioned the 10% drop in metabolism. I wish someone had told me sooner. Now I track my steps and protein intake religiously. It’s not perfect, but I’m stable. You’re not lazy-you’re medicated.
Adrian Rios
Let’s be real here-this whole system is broken. We’ve got drugs that can make you lose 15% of your body weight, but doctors still hand out olanzapine like candy to people with schizophrenia and then act surprised when they develop type 2 diabetes. It’s not just ignorance-it’s institutional neglect. The FDA’s new labeling requirements are a start, but we need mandatory metabolic screening before prescribing anything that touches your appetite or insulin. This isn’t about willpower-it’s about pharmacology being treated like a blunt instrument instead of a scalpel.
Casper van Hoof
The notion that weight gain is an unintended consequence presumes an anthropocentric view of pharmacological intent. In truth, the body is not a vessel to be optimized, but a dynamic system responding to molecular stimuli. To pathologize weight change is to mistake physiology for morality. The real question is not whether drugs cause weight gain-but whether society is prepared to accept biological truth over aesthetic preference.
Richard Wöhrl
Just wanted to add-GLP-1s aren’t just for weight loss anymore. I’m on semaglutide for diabetes, and my doctor just added it because my insulin was making me gain 3 lbs/month. It’s wild how it cuts cravings so hard-I stopped snacking at 2 a.m. without even trying. Also, if you’re on any antipsychotic, ask for the HTR2C test. Mine said I was high-risk for weight gain on olanzapine. Switched to lurasidone. Lost 11 lbs in 4 months. No magic. Just science.
Pramod Kumar
Bro, I was on risperidone and gained 20 kilos in 8 months. My mom said I looked like a different person. I cried every time I saw my reflection. Then I switched to ziprasidone-zero weight gain, same mental clarity. People think mental health meds are a trade-off. They’re not. There are better options. You just gotta ask. And if your doc says 'it's fine'-go get a second opinion. Your body deserves better than a guess.
Brandy Walley
Wow so now we’re treating weight gain like a medical emergency? Next they’ll make us sign a waiver before taking Tylenol. I gained 5 lbs on antidepressants and guess what-I’m still alive. People need to chill. You’re not a scale. You’re a human. Stop letting Big Pharma scare you into switching meds you actually need.
shreyas yashas
My uncle was on insulin for 10 years, gained 40 kg. Then he tried semaglutide. Lost it all. Now he hikes every weekend. No magic. Just the right tool. If your doctor doesn’t know about GLP-1s, find one who does.
Suresh Ramaiyan
There’s a quiet tragedy here: we treat the mind and ignore the body. But the body remembers. The weight gain isn’t just fat-it’s shame, it’s isolation, it’s the erosion of self-worth. Healing isn’t just about the right drug. It’s about being seen. Maybe the real medicine isn’t in the pill-it’s in the conversation we’re finally having.
Katy Bell
I switched from paroxetine to bupropion and lost 8 lbs in 3 months without trying. My anxiety didn’t get worse. My skin cleared up. I started wearing shorts again. I just wish someone had told me this was an option before I spent a year hating my reflection.
Ragini Sharma
so i asked my dr if my mood meds were making me fat and she said ‘well maybe u just like food now lol’… like… i’m not a joke. i’m on 3 meds and my jeans are in the donation bin. thanks for the laugh doc.