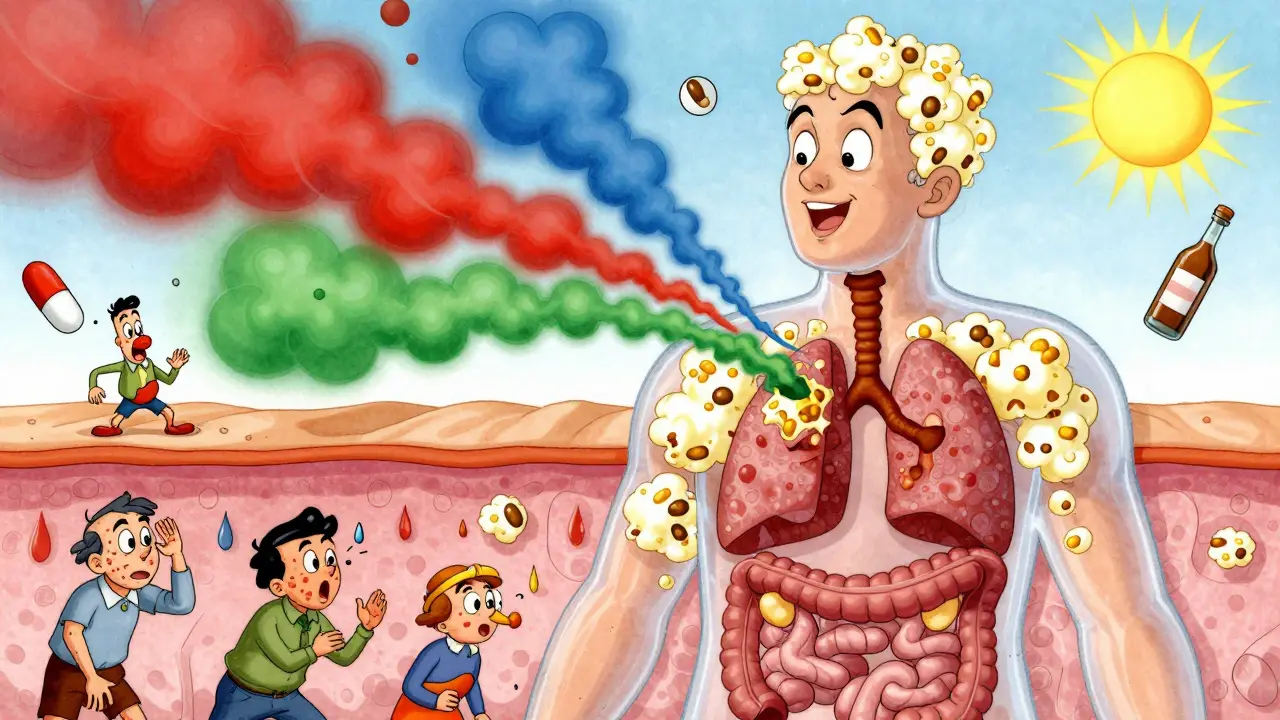
When your body reacts to something harmless-like pollen, a food, or even stress-and you break out in hives, feel dizzy, get stomach cramps, or have trouble breathing, it’s not always an allergy in the classic sense. More often, it’s your mast cells going into overdrive. These tiny immune cells, first spotted by Paul Ehrlich in 1878, live in your skin, lungs, gut, and other places where your body meets the outside world. They’re supposed to guard you from invaders. But when they activate too easily or too often, they dump out a storm of chemicals that make you feel awful. This isn’t just hay fever. It’s Mast Cell Activation Syndrome (MCAS), a condition affecting up to 1 in 1,000 people.
What Happens When Mast Cells Activate?
Mast cells don’t just explode randomly. They respond to specific triggers. The most common is IgE antibodies sticking to allergens like peanut proteins or bee venom. That’s the classic allergy pathway. But there are dozens of other ways they can get triggered: bacterial parts, heat, pressure, emotional stress, NSAIDs like ibuprofen, alcohol, and even certain foods. In fact, a 2022 survey of over 1,200 MCAS patients found that 68% react to NSAIDs, 63% to alcohol, and 57% to heat.
Once triggered, mast cells release chemicals in two waves. The first wave-within seconds-is made of pre-stored mediators. These include histamine (which causes itching, swelling, and low blood pressure), tryptase (a marker doctors test for), chymase, and heparin. These are packed into granules inside the cell like a bomb waiting to go off. When the signal comes, the cell opens up and spills them out all at once. That’s why symptoms like flushing, hives, or sudden nausea can hit so fast.
The second wave takes minutes to hours. These are newly made chemicals: prostaglandin D2, leukotriene C4, and a long list of cytokines like TNF-alpha and IL-6. These don’t just cause immediate symptoms-they keep inflammation going for hours or even days. That’s why some people with MCAS feel wiped out, foggy, or achy long after the initial reaction. Unlike antihistamines, which only block histamine, these later mediators are behind the fatigue, brain fog, and chronic pain many patients struggle with.
Why Mast Cell Stabilizers Are Different
Most allergy meds-like loratadine or cetirizine-try to clean up the mess after it’s made. They block histamine receptors so the chemical can’t bind and cause symptoms. But if the mast cell is still releasing histamine, tryptase, prostaglandins, and cytokines, you’re only treating one piece of a big puzzle.
Mast cell stabilizers work upstream. They don’t block receptors. They stop the cell from releasing anything in the first place. The most well-known is cromolyn sodium, approved by the FDA in 1973. It works by preventing calcium from flooding into the mast cell. Without that calcium signal, the granules don’t fuse with the cell membrane, and nothing gets released. Ketotifen, another stabilizer approved in the U.S. in 1990, does something similar but also has mild antihistamine effects.
Here’s the catch: these drugs don’t work if you take them after symptoms start. They’re prophylactic. You need to take them before you’re exposed to a trigger. A patient who eats a trigger food without taking cromolyn will still react. But if they take it 30-60 minutes beforehand, their reaction might be mild or nonexistent.
Studies show cromolyn sodium reaches peak levels in the blood within 2-4 hours after oral dosing, with a half-life of just 1.5 hours. That’s why most people need to take it four times a day-morning, midday, afternoon, and bedtime. The standard starting dose is 100 mg four times daily, slowly increasing to 200-400 mg four times daily over weeks. Some patients report 70% fewer anaphylactic episodes after hitting the right dose, but it takes time. One documented case showed improvement only after eight weeks.
What Works and What Doesn’t
Mast cell stabilizers aren’t magic bullets. They don’t stop cytokine production entirely. Even if degranulation is blocked, the cell can still make new inflammatory signals through other pathways. That’s why many patients still feel fatigued or have brain fog despite taking cromolyn.
Response rates vary. About 40-60% of MCAS patients see some benefit from stabilizers. Compare that to newer biologics like omalizumab (an anti-IgE drug), which helps 70-80% of patients. But omalizumab costs thousands per month and requires monthly injections. Cromolyn, by contrast, is generic, cheap, and taken orally.
Side effects are real. A 2021 Drug Safety study found 35% of cromolyn users had nausea or diarrhea, and 15% quit because of it. The liquid form tastes awful-rated just 2.1 out of 5 in patient surveys. That’s why some kids need it given through feeding tubes. Newer formulations and capsules are helping, but palatability remains a barrier.
And here’s something patients rarely hear: stabilizers don’t fix everything. If your mast cells are activated by stress or heat, you can’t take a pill before you step into the sun or have a bad day at work. That’s why managing triggers is just as important as taking medication.
The Trigger Wheel: Real-Life Culprits
Many MCAS patients use what’s called the “mast cell trigger wheel.” It’s a visual tool that maps out common triggers. The biggest ones, based on patient surveys, are:
- NSAIDs (ibuprofen, aspirin) - 68%
- Alcohol - 63%
- Heat - 57%
- Emotional stress - 52%
- Specific foods (aged cheese, shellfish, citrus, tomatoes) - 49%
- Perfumes and strong odors - 45%
- Exercise - 41%
Some triggers are obvious. Others aren’t. A hot shower, a crowded room, or even a change in barometric pressure can set off a reaction. That’s why keeping a detailed symptom diary is crucial. Patients who track what they ate, where they were, what they felt, and what meds they took are far more likely to spot patterns and avoid triggers.
Diagnosis Is Hard-But Getting Better
It takes most people 6 to 10 doctor visits over 3 to 5 years to get diagnosed with MCAS. Many are told they have anxiety, IBS, or chronic fatigue syndrome. That’s because the symptoms overlap so much.
Diagnosis relies on three things: recurring symptoms affecting two or more body systems (skin, gut, lungs, cardiovascular), improvement with mast cell-targeted meds, and lab evidence of mediator release. Doctors test for:
- Serum tryptase (must be ≥20% above baseline + 2 ng/mL above normal)
- 24-hour urinary methylhistamine (normal <1.3 mg)
- N-methyl-β-hexosaminidase (normal <1,000 ng/mg creatinine)
Successful treatment means a 30% drop in these markers. But not all clinics agree on the criteria. Some follow strict lab standards. Others, like the AAAAI, say if symptoms improve with stabilizers and you rule out other causes, you can diagnose MCAS clinically.
Genetics play a role too. About 30% of MCAS patients have mutations in genes like KIT, TPSAB1, or CBL. These affect how mast cells grow and respond. That’s why some people are more sensitive than others.
What’s Next?
The field is moving fast. In 2023, the FDA approved avapritinib for advanced systemic mastocytosis, a related but more severe condition. It targets the KIT D816V mutation, which drives abnormal mast cell growth. Early results show a 60% response rate.
Even more promising are drugs in development. SYK kinase inhibitors, currently in Phase II trials, have shown 75% reduction in mediator release at 100 mg daily. These could be game-changers-targeting multiple pathways at once, not just degranulation.
By 2030, experts predict next-gen therapies will help 80-90% of MCAS patients achieve near-complete symptom control. Until then, mast cell stabilizers remain the most accessible, affordable tool we have.
Practical Tips for Starting Stabilizer Therapy
If you’re considering cromolyn or ketotifen:
- Start low: 100 mg four times daily with meals and at bedtime.
- Give it time: Don’t expect results in a week. Wait at least 6-8 weeks.
- Track triggers: Use a symptom journal or app to log food, stress, temperature, and reactions.
- Avoid NSAIDs and alcohol: These are top triggers-cut them out first.
- Test your markers: Ask your doctor for baseline and follow-up tests for tryptase and urinary methylhistamine.
- Don’t give up if you have side effects: Try a different formulation or take with food. Some patients do better with capsules than liquid.
Support groups like the Mast Cell Disease Society and Reddit’s r/mcas have over 20,000 members combined. They share dosing tips, trigger lists, and doctor recommendations. You’re not alone.
Can mast cell stabilizers cure MCAS?
No, mast cell stabilizers don’t cure MCAS. They help control symptoms by preventing mast cells from releasing too many mediators. MCAS is a chronic condition, and most patients need long-term management. Some people can reduce doses over time, but many require ongoing treatment to stay stable.
How long does it take for cromolyn sodium to work?
It usually takes 4 to 8 weeks to see noticeable improvement. Some patients report minor changes in the first week, but full benefit often takes two months. Patience is key-this isn’t a quick fix like an antihistamine. Consistent dosing is essential.
Are mast cell stabilizers safe for long-term use?
Yes. Cromolyn sodium and ketotifen have been used safely for decades. Long-term studies show no major organ toxicity. The main issues are gastrointestinal side effects-nausea, diarrhea-which often improve with time or dose adjustment. Regular monitoring by a specialist is still recommended.
Can I take mast cell stabilizers with antihistamines?
Yes, and many patients do. Antihistamines block histamine after it’s released, while stabilizers prevent the release in the first place. Using both gives you a two-layer defense. H1 blockers like loratadine and H2 blockers like famotidine are commonly combined with cromolyn for better symptom control.
Why do some doctors not believe in MCAS?
MCAS was only formally recognized in 2010, and diagnostic criteria are still evolving. Many doctors were trained to think of allergies as IgE-mediated only. MCAS involves multiple triggers and mediators, which doesn’t fit the old model. Also, symptoms overlap with anxiety, IBS, and fibromyalgia. But as more research emerges and patient numbers grow, awareness is improving. About 78% of academic medical centers now have dedicated mast cell clinics.

Chiraghuddin Qureshi
OMG this is so me 😭 I thought I was just 'weirdly sensitive' until I read this. Heat + alcohol = instant hives and brain fog. Took me 7 years to find out it wasn't 'anxiety'. Cromolyn saved my life. 🙏
Patrick Roth
Actually, most of this is pseudoscience. Mast cell activation syndrome isn't even officially recognized by the WHO. You're just describing people with anxiety disorders who found a fancy label. Tryptase levels are normal in 90% of these 'patients'.
Kenji Gaerlan
cromolyn tastes like ass. i took it for 3 weeks. got diarrhea every time. my kid had to get it through a feeding tube. no thanks. i'd rather just avoid cheese and coffee and call it a day.
Oren Prettyman
It is imperative to underscore the methodological deficiencies inherent in the cited 2022 survey, which lacks a control cohort, employs self-reported data without biochemical verification, and fails to account for confounding variables such as concomitant histamine intolerance or concurrent medication use. The causal attribution to mast cell degranulation is thus not only speculative but potentially misleading to the lay reader.
Tatiana Bandurina
You say 'up to 1 in 1,000' but you cite a survey of 1,200 patients. That's not population data. That's a self-selected online group. You're pathologizing normal human variation. Also, why are you promoting a drug with a 35% GI side effect rate as a first-line solution? This reads like pharmaceutical marketing.
Sarvesh CK
The complexity of mast cell biology is both fascinating and humbling. While stabilizers like cromolyn offer a mechanistic approach to modulating degranulation, one must also consider the broader neuro-immune axis-how chronic stress, gut dysbiosis, and environmental toxins may prime mast cells for hyperreactivity. A holistic framework, integrating dietary modulation, vagal toning, and circadian alignment, may yield more sustainable outcomes than pharmacological intervention alone.
Brenda King
I’ve been on cromolyn for two years. It’s not perfect but it’s the only thing that keeps me from collapsing after a hot shower or a glass of wine. I used to think I was just weak. Turns out I have a biological condition. This post got me crying in the grocery store. Thank you for explaining it so clearly. 💙
Keith Helm
Cromolyn doesn't cross the blood-brain barrier. Therefore, it cannot address brain fog. Your claim is biologically implausible.
Daphne Mallari - Tolentino
One must question the academic rigor of a condition that relies so heavily on patient-reported trigger wheels and anecdotal correlation. The absence of a gold-standard diagnostic biomarker renders MCAS a construct of contemporary medical fashion, not evidence-based science.
Neil Ellis
This post is like a love letter to people who’ve been told they’re crazy for 10 years. I used to hide my reactions-flushing in the elevator, collapsing after sushi, crying because a perfume made me feel like I was dying. Now I carry my cromolyn like a superhero’s power-up. It’s not magic, but it’s mine. And I’m not broken. I’m just wired differently. 🌈
Rob Sims
So you're telling me people who can't handle spicy food or stress are now 'patients'? Next you'll be diagnosing 'gluten sensitivity' because someone got bloated after pizza. This is medical gaslighting dressed up as science.
arun mehta
As someone from India where Ayurveda has long recognized 'Vata imbalance' as a root of systemic reactivity, I find it deeply validating to see Western medicine finally catching up. The trigger wheel mirrors doshic aggravation patterns-heat, stress, and certain foods disrupt our inner equilibrium. Perhaps the future lies in integrating ancient wisdom with modern pharmacology, not dismissing either.
Lauren Wall
I’m not even mad, I’m just disappointed. You wrote a 2000-word essay on a drug that doesn’t work for most people and didn’t mention low-histamine diets once.