Duloxetine Liver Risk Assessment Tool
Assess Your Liver Risk
This tool helps you understand your individual risk of liver injury while taking duloxetine based on key factors. Remember, most people tolerate duloxetine without liver issues, but certain factors increase risk.
Your Risk Assessment
Recommended Testing Timeline
Baseline Test (Before Starting)
Recommended for all patients before starting duloxetine
8-12 Weeks After Starting
Most important monitoring time for liver injury
Repeat Tests Every 3-6 Months
Recommended for high-risk patients
What to Watch For
- Unexplained fatigue
- Nausea or loss of appetite
- Itching without a rash
- Dark urine
- Pale stools
- Yellowing of skin or eyes (jaundice)
- Pain in upper right abdomen
When you start taking duloxetine for depression, anxiety, or chronic pain, your mind is focused on how it will make you feel-less overwhelmed, less tired, less in pain. But there’s a silent risk that doesn’t show up in mood logs or pain scales: duloxetine can harm your liver. It’s rare, but it happens. And if you don’t know the signs or when to get tested, you could miss the warning signs until it’s too late.
Why Duloxetine Can Affect Your Liver
Duloxetine, sold under the brand name Cymbalta, is a serotonin-norepinephrine reuptake inhibitor (SNRI). It works well for depression, generalized anxiety, diabetic nerve pain, and fibromyalgia. But unlike some other antidepressants, it’s processed by your liver using enzymes called CYP1A2 and CYP2D6. These enzymes break down the drug, but sometimes they create small, reactive byproducts that can damage liver cells. This isn’t a problem for most people. But for some, even at standard doses (30-60 mg daily), the liver can’t handle the load. The risk goes up when you increase the dose from 30 mg to 60 mg-something many doctors do after a week if symptoms don’t improve. That’s when liver enzyme spikes are most likely to happen. Studies show that about 1-2% of people on duloxetine develop mild liver enzyme elevations. In about 0.6% of cases, ALT (alanine aminotransferase) levels rise more than three times the normal upper limit. That’s not just a lab number-it’s a signal your liver is under stress.When Does Liver Damage Show Up?
There’s no set timeline, but the pattern is clear: most cases of duloxetine-related liver injury appear between 35 and 62 days after starting the drug. The median time? Around 50 days. That’s why waiting three months for a routine checkup isn’t enough. If you started duloxetine in January, you should be thinking about liver health by late February. This isn’t about paranoia-it’s about timing. The damage often starts quietly, without symptoms. By the time you feel tired, nauseous, or notice yellow eyes, the injury may already be advanced. Case reports show people with no prior liver issues-no alcohol use, no hepatitis, no obesity-suddenly developing ALT levels over 700 U/L (19 times the normal limit). One patient on Drugs.com needed hospitalization after 45 days on 60 mg. Another took it for five years with only minor, harmless spikes. It’s unpredictable. That’s why monitoring isn’t optional-it’s essential.Who’s at Higher Risk?
You might think only heavy drinkers or people with cirrhosis are at risk. But that’s outdated thinking. While duloxetine is contraindicated in people with chronic liver disease, most cases happen in people who seem perfectly healthy. Still, some factors raise your odds:- BMI of 30 or higher (obesity)
- Diabetes
- Drinking more than 14 drinks a week (men) or 7 drinks a week (women)
- Taking other medications that stress the liver-like statins, NSAIDs, or certain antibiotics
- Being a poor metabolizer of CYP2D6 (a genetic trait that slows drug breakdown)
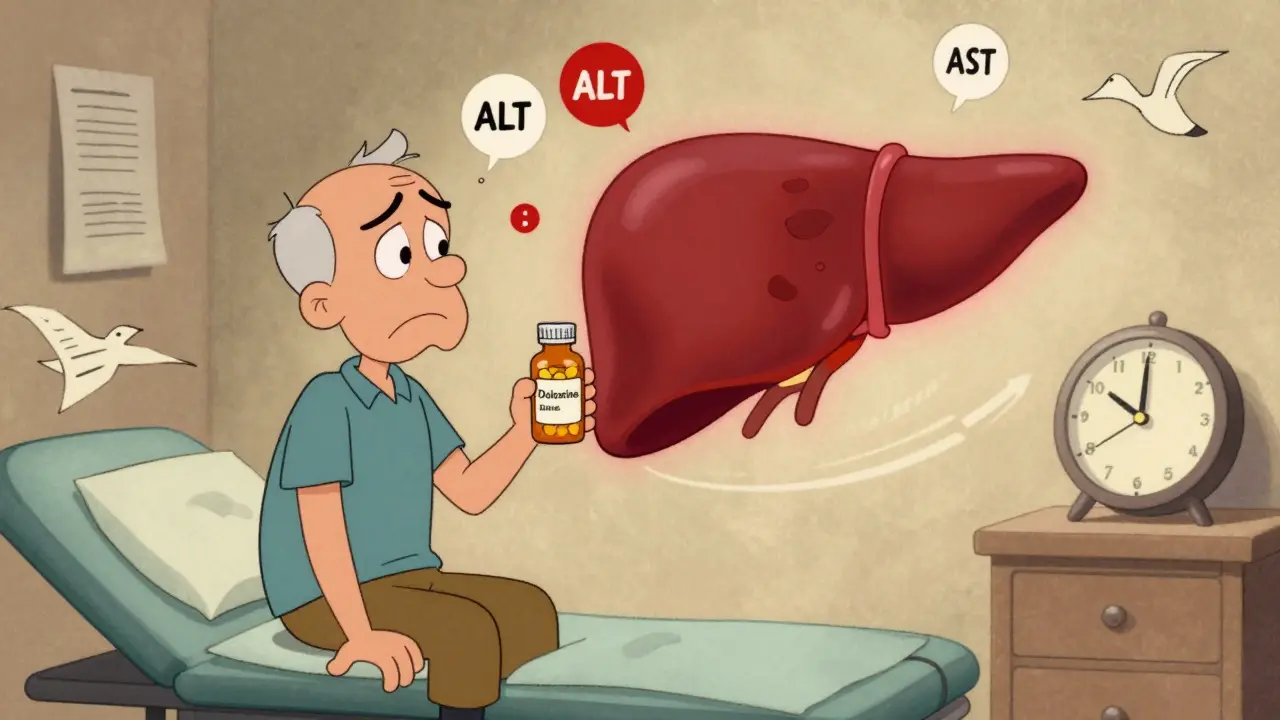
What Tests Should You Get?
Don’t wait for symptoms. Get tested before you start and again within 8-12 weeks. The key blood tests are:- ALT (alanine aminotransferase)
- AST (aspartate aminotransferase)
- Alkaline phosphatase
- Total bilirubin
What Happens If Liver Enzymes Rise?
It’s not a death sentence. Most cases reverse completely if caught early. Here’s what to do based on your numbers:- ALT or AST 3-5x ULN, no symptoms: Repeat the test in 1-2 weeks. If it’s still high or rising, stop duloxetine and talk to your doctor about alternatives.
- ALT or AST >5x ULN, or any symptoms: Stop the drug immediately. Symptoms include dark urine, yellow skin or eyes, severe fatigue, nausea, vomiting, itching, or right-side abdominal pain.
- After stopping: Don’t quit cold turkey. Taper slowly over 2-4 weeks to avoid withdrawal like dizziness, brain zaps, or anxiety spikes. Your doctor should guide this.
How Does Duloxetine Compare to Other Antidepressants?
Not all antidepressants carry the same liver risk.- SSRIs (like sertraline, fluoxetine): Lower risk. Only about 0.5% of users have ALT elevations above 3x ULN.
- Other SNRIs (like venlafaxine): Similar risk to duloxetine. About 1.7x higher than SSRIs.
- Tricyclics (like amitriptyline): Higher risk of heart issues, but lower liver risk than SNRIs.
- Bupropion: Low liver risk, but can lower seizure threshold.
What Patients Are Saying
Online forums are full of mixed experiences. On Reddit, a psychiatrist with 8 years of experience said she’s seen three cases of serious liver injury-all between days 35 and 62. All patients recovered after stopping duloxetine. On Drugs.com, one user wrote: "I was told it was safe. No one mentioned my liver. By the time I turned yellow, I was in the ER." Another said: "I’ve been on it for 5 years. My liver’s fine. I get tested every 3 months. That’s all it takes." A review of 1,247 WebMD reviews found that 63% of negative comments mentioned unexpected liver side effects. That’s a red flag. Many patients weren’t warned.
What Doctors Are Doing Now
The FDA doesn’t require routine liver tests for duloxetine. But that’s changing. In 2023, the FDA issued draft guidance pushing for standardized monitoring of all drugs linked to liver injury. The American College of Gastroenterology is expected to release new guidelines by late 2024-likely recommending baseline LFTs for all SNRI users. Right now, best practice is clear:- Test liver enzymes before starting duloxetine.
- Test again at 8-12 weeks, especially if you’re overweight, diabetic, or on other meds.
- Know the symptoms of liver trouble.
- Don’t assume you’re fine just because you feel better mentally.
What You Should Do
If you’re taking duloxetine:- Ask your doctor for a baseline liver panel before you start, or if you haven’t had one yet.
- Request a repeat test at 8-12 weeks. Don’t wait for your next depression checkup.
- Write down symptoms: fatigue, nausea, itching, dark urine, yellow skin.
- If you’re on other medications, make sure your doctor knows. Some drugs stack up on the liver.
- Don’t panic if your ALT is slightly high. But don’t ignore it either.
- Ask: "Do you test liver enzymes before prescribing this?" If the answer is no, ask why.
- Discuss alternatives if you have risk factors like obesity or diabetes.
- Remember: your mental health matters-but so does your liver.
Final Thought
Duloxetine is a powerful tool. It helps millions. But like any medicine, it comes with trade-offs. The liver doesn’t complain until it’s too late. That’s why checking your numbers isn’t just good practice-it’s the difference between managing a side effect and facing a medical emergency. You’re not being paranoid. You’re being smart.Can duloxetine cause permanent liver damage?
In most cases, no. If duloxetine-induced liver injury is caught early and the drug is stopped, liver enzymes return to normal within weeks to months. There are rare reports of severe injury requiring hospitalization, but permanent damage or liver failure is extremely uncommon-fewer than 1 in 10,000 users. The key is early detection. Once you stop taking duloxetine, the liver usually repairs itself.
Do I need liver tests if I’m taking 30 mg of duloxetine?
Yes. While the risk is lower at 30 mg, cases of liver injury have been reported even at this dose. The median time to enzyme elevation is around 50 days, regardless of starting dose. Baseline testing is recommended for everyone. If you stay at 30 mg and feel fine, you may not need a repeat test unless you develop symptoms or add other medications.
Can I take duloxetine if I’ve had hepatitis in the past?
If you have chronic liver disease, cirrhosis, or active hepatitis, duloxetine is contraindicated. The FDA warns against its use in these cases because your liver can’t process it safely-exposure levels can be up to 7 times higher than normal. If your hepatitis was cured years ago and your liver function is now normal, talk to your doctor. You may be able to use it with close monitoring, but only after a full liver evaluation.
What are the early signs of liver damage from duloxetine?
Early signs are often subtle: unexplained fatigue, loss of appetite, mild nausea, or itching without a rash. These can be mistaken for depression or side effects of the drug itself. More obvious signs include dark urine, pale stools, yellowing of the skin or eyes (jaundice), and pain in the upper right abdomen. If you notice any of these, stop taking duloxetine and contact your doctor immediately.
Are there safer antidepressants for people with liver concerns?
Yes. SSRIs like sertraline, escitalopram, and citalopram have a lower risk of liver injury compared to duloxetine and other SNRIs. Bupropion is another option with minimal liver impact, though it carries other risks like seizures in susceptible people. If you have risk factors like obesity, diabetes, or alcohol use, your doctor may start you on an SSRI instead. Always discuss alternatives before starting any new medication.
How often should I get liver tests if I’m on duloxetine long-term?
For most people, one follow-up test at 8-12 weeks is enough. If your liver enzymes are normal and you have no risk factors, annual testing is usually sufficient. If you have risk factors-like obesity, diabetes, or are on other liver-affecting drugs-every 3-6 months is recommended. Always get tested if you start a new medication or if you develop symptoms like fatigue or jaundice.

Steve Hesketh
I was on duloxetine for 8 months for anxiety and never knew about the liver risk. My doctor never mentioned it. I felt fine mentally, but I was always tired and had this weird itch. Turns out my ALT was 210. They pulled me off it and I'm fine now. I'm so glad I found this post. You're doing important work here.
Don't let anyone tell you it's 'just depression'-your liver doesn't care about your mood. It just wants to live.
shubham rathee
this is all just big pharma fearmongering they want you to get tested so they can sell you more drugs and labs make money off blood work the real cause is processed food and glyphosate in your water dont trust your doctor theyre paid by cymbalta
Melanie Pearson
The American Psychiatric Association does not mandate routine liver enzyme monitoring for SNRIs. This post overstates the risk and misrepresents clinical guidelines. While vigilance is prudent, conflating mild enzyme elevations with hepatotoxicity is alarmist and potentially harmful to patient adherence. The data does not support routine testing for low-risk individuals.
Barbara Mahone
I'm a nurse in Chicago and I've seen this twice in the last year. Both patients were on 60mg, both had type 2 diabetes, both were asymptomatic until their labs came back. One had ALT over 700. Neither had been tested before starting.
It's not paranoia. It's basic care. I wish more people knew this.
Kelly McRainey Moore
I started duloxetine last year and got my liver checked at 6 weeks. Everything was normal. I just wanted to share that it’s not scary if you’re proactive. My doctor was super chill about it and just said, 'Let’s keep an eye.' And that’s all you need.
Amber Lane
My mom had liver damage from duloxetine. She was 68, no alcohol, no obesity. Just took it for 50 days. Never knew until she turned yellow. Don't wait for symptoms.
Roisin Kelly
Why do they never warn you? I was on it for 3 years. My doctor said 'it's fine' until my bilirubin hit 4.8. Then he acted like it was my fault for not asking. You know what? I didn't know to ask because NO ONE TOLD ME. This is medical gaslighting.
Samuel Mendoza
SSRIs cause more liver damage than SNRIs. The data is clear. This article is misleading.
Yuri Hyuga
I’ve been a psych nurse for 12 years and I’ve seen this exact pattern repeat: healthy person, feels better mentally, gets lazy about labs… then boom. Liver’s fried.
It’s not about fear. It’s about responsibility. Your brain deserves care. So does your liver. 🫂❤️🩹
Coral Bosley
I’m a pharmacist and I’ve seen people get liver transplants from this. Not because they were drunks or junkies-because they were moms and teachers and college students who trusted their doctors. You think your liver is invincible? It’s not. It’s a silent warrior. And it’s begging you to listen.
MAHENDRA MEGHWAL
The data presented is scientifically accurate and clinically relevant. Baseline and follow-up liver function tests are not merely recommended-they are ethically imperative for all patients initiating duloxetine, particularly in populations with metabolic comorbidities. This post serves as a necessary corrective to the prevailing negligence in psychiatric prescribing practices.